WHAT THE SCIENCE IS TELLING US
The following report concludes a 6 month investigation through the National Library of Medicine in an attempt to identify the current state of knowledge regarding the rapid rise being observed in diabetes in adults and children. In just a moment, you'll read studies from Harvard, University of Illinois, Princeton, Tennessee State, the National Institutes of Health and many other reputable research facilities all finding the same common denominator: People with either type-1 or type-2 diabetes are consistently found to have higher blood levels and exposures to specific chemicals from common everyday consumer products and lifestyle choices. These chemicals are reported to cause disruptions in gene expression - subtle weakening to the immune system - autoimmunity - copying of natural hormones and damage to the thymus gland (which protects all of us from diabetes and health disorders related to diabetes). This new information provides the logic and foundation for accelerating research into new directions for treatment, some of which have begun and are showing unprecedented reversal of diabetes. This investigative project has been a combined effort between Richard Pressinger and other researchers who believe it is essential this information be made accessible to physicians, the media and general public. Richard Pressinger holds a Masters Degree in Education from University of Florida and was motivated to begin this project after his son Alan, at age 12, developed type-1 diabetes in May 2016.
INTRODUCTION
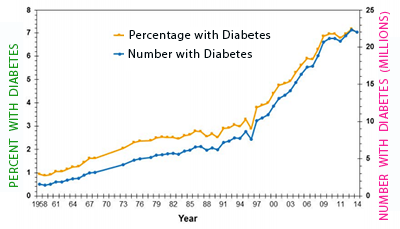
 The percentage of the U.S. population with diabetes has increased dramatically over the past 20 years and is increasing faster with each passing year. In the following report, we will provide clear and convincing evidence that the main force driving the rising rates of diabetes is not an increasing elderly population or the increase in obesity, but is occurring from something else.
The percentage of the U.S. population with diabetes has increased dramatically over the past 20 years and is increasing faster with each passing year. In the following report, we will provide clear and convincing evidence that the main force driving the rising rates of diabetes is not an increasing elderly population or the increase in obesity, but is occurring from something else.
Most people believe the increase in diabetes is occurring because people are simply eating more and becoming obese. Seems like a plausible explanation since obese people do have higher rates of diabetes. However, scientists studying diabetes found evidence showing it is not that simple. In fact, when researchers studied blood samples of 2,016 adults from the 1999-2002 National Health and Examination Survey, they found a fascinating pattern: Some people with obesity had very low rates of diabetes while others with obesity had extremely high rates of diabetes. So what was going on? It turns out these higher rates of diabetes had nothing to do with exercise or eating patterns, but everything to do with having high levels of six different chemicals in their blood. In fact, people with the highest levels of these six chemicals had a whopping 38-fold increase rate of diabetes. For the sake of understanding the magnitude of this, for every 1 out of 100 people who had diabetes and low levels of these 6 chemicals, there were 38 people out of 100 who had diabetes if they had the highest levels of these 6 chemicals. This is why it is called a 38-fold increase. Having high levels of these six chemicals would depend on things such as specific consumer product choices - when their house was built - where their house was located - their driving habits - and choices of construction workers building the house as well as choices made by residents who lived in the house before them. Getting interesting isn't it? In fact, when the scientists analyzed the numbers, people whose bodies had the highest 10% of these six chemicals had the 38 times greater risk of diabetes than those in the group with the lowest 25% of these six chemicals. After understanding this study, anyone who thinks that obesity is still the main reason for the diabetes increase most certainly need to take a math refresher course at their local junior college.
Although the details of this study will be discussed in upcoming pages, some of you at this moment may be experiencing a bit of disbelief. If this is you, we'd like to gain your confidence for our future discussions, so please take a moment and confirm the research we just discussed. This can be done by going to the National Institutes of Health medical journal listing website at "www.pubmed.gov" - Once there, type in the following journal name, volume number and pages. This diabetes/obesity/chemical study we reviewed was published in the July 2006 journal Diabetes Care, Volume 29(7), pages 1638-1644. If you are reading this online, you can view the study from this link.
What we've learned from this study is that the obesity/diabetes connection is not as cut and dry as previously thought. The connection between the diabetes explosion and obesity weakens further still when we realize that the fastest growing group for diabetes is not among those who are overweight, but is happening to our youngest children of normal weight. White caucasian children under age 5 are experiencing an increase in diabetes that is faster than any other age group or nationality.
IS IT THE OLD FOLKS?
If the major push behind the rise in diabetes is not from obesity, what else could it be? The first thing that comes to mind should be the increase numbers of people in our aging population. This also makes sense since the risk of type-2 diabetes increases as we get older. So, to determine if aging is responsible for the diabetes epidemic all we need to do is to look at the number of people with diabetes for those who are in their 70's and 80's. If aging were the culprit, the diabetes rates would be increasing there and not in younger ages. So, when checking the numbers what do we see? Yes, the number and percent of people with diabetes is increasing for those in their 70's. But the funny thing is, the percent with diabetes is also increasing for people in their 60's - and 50's - and 40's - and 30's - and 20's and even in children age 10 to 18. It is increasing for people who are obese and among people who are not obese. Do I have your attention yet?
SHOULD WE LISTEN TO THE SCIENTISTS?
In a few moments you'll read conclusions from research conducted by Harvard, University of Illinois, Princeton, Tennessee State, the National Institutes of Health and many other reputable research facilities around the world showing a very disturbing pattern; People who develop diabetes are being found to have higher blood levels and exposures to specific chemicals in common everyday consumer products and lifestyle choices. These chemicals then cause disruptions in gene expression - subtle weakening to the immune system - autoimmunity - copying of natural hormones and damage to the thymus gland (which protects all of us from diabetes and health disorders related to diabetes). In fact, the number of medical and scientific studies linking modern chemicals with diabetes had increased to such an extent by 2010, that the National Institutes of Health held an international workshop from January 11-13, 2013 to bring together scientists from around the world to specifically address the diabetes/chemical connection. A summary of their "workshop" was published in the journal Environmental Health Perspectives: Vol. 120(6), June 2012. Along with presentations by scientists linking diabetes with exposure to specific types of chemicals found in everyday consumer products, another conclusion was strong support for the "developmental obesogen" hypothesis, which suggests that chemical exposures can increase the risk of obesity (and I'm quoting their report here) - "by altering the differentiation of adipocytes (fat cells) or the development of neural circuits that regulate feeding behavior." To put this another way - many of the same chemicals now linked to diabetes are also being found to "fool" hormones in the body and cause increases in body weight and obesity.
All of this supports the argument that obesity and aging are not the main culprits behind the diabetes epidemic, but that something else is going on, and that "something else" must be discussed and acted upon no matter how much we dislike admitting we've been doing something wrong for so many years. Momentum doesn't make something right and people don't like change, I get that, but failure to address and correct these issues immediately will result in truly dire consquences for us and our children in the very near future.
In my 62 years on this planet I've come to the conclusion that there are two types of people, those who care only about the present and those who care about the future. If you consider yourself part of the latter, we need your help as time is literally running out as we're almost at the point of no-return.
To provide you with the latest findings from scientific research from the National Library of Medicine, we have created concise summaries of this research in an easy to read and comprehensive format. To insure accuracy of all information - each journal summary includes the journal name, date and research centers involved in the study along with a link to the original journal article in the far right column. We begin with a discussion into the latest numbers and why we believe diabetes will be the first to literally break the back of modern society.
DIABETES RATES
INCREASING DRAMATICALLY
IN U.S.
 Here's some numbers that should wake you up - when looking at the latest numbers from 2012, researchers found that 14% of the adult U.S. population had either doctor diagnosed diabetes or undiagnosed diabetes. Also using 2012 numbers, the American Diabetes Association states that 38% of us have a condition known as prediabetes, which is a nice way of saying the person will most likely have diabetes in 5-10 years. Putting these two numbers together, the American Diabetes Association is telling us that close to 50% of the U.S. population has diabetes or prediabetes now and about 40% of our population will have full diabetes sometime before 2022.
Here's some numbers that should wake you up - when looking at the latest numbers from 2012, researchers found that 14% of the adult U.S. population had either doctor diagnosed diabetes or undiagnosed diabetes. Also using 2012 numbers, the American Diabetes Association states that 38% of us have a condition known as prediabetes, which is a nice way of saying the person will most likely have diabetes in 5-10 years. Putting these two numbers together, the American Diabetes Association is telling us that close to 50% of the U.S. population has diabetes or prediabetes now and about 40% of our population will have full diabetes sometime before 2022.
The fact that diabetes was only 1% in 1960 and continues to increase rapidly today, paints a very sad and disturbing picture for our childrens' future, but you should also be very concerned for yourself. The way numbers are increasing yearly, if you don't have diabetes or prediabetes now, you probably will in the next 5, 10 or 15 years - and the baggage of health disorders, pain and suffering that comes with it, well, you wouldn't wish on your worst enemy.
WHAT IS DIABETES - A BIOLOGY LESSON
A quick biology lesson in case you are not familiar with diabetes. First, you need to understand there are two types of diabetes. One is conveniently called type-1 and the other is type 2. Both have one thing in common - the human body is having problems getting the fuel known as glucose into our cells. Glucose is basically the gasoline that keeps the cells in your body and brain running. To make it simple, if our cells cannot get the glucose they need - our brain has a hard time thinking and our muscles have a difficult time working. If cells continue getting less and less glucose - we can lose consciousness and go into a diabetic coma. If this process continues, we eventually die. In fact, this is exactly what happened to children with diabetes before insuliln was discovered in 1921 and will be explained later as it is truly a heart-warming story.
TWO TYPES OF DIABETES - SAME RESULT
While both types of diabetes show their ugly faces when we are unable to get enough glucose into the cell - why this happens in type 1 is quite different than why it happens with type 2. The irony of diabetes is there is plenty of glucose in the blood, but the cells cannot use the gluocse that surrounds them. So herein lies the problem - glucose is apparently a stubborn little fellow and refuses to go into the cell by itself. It will only enter the cell if escorted by its friend known as insulin. You could say that insulin is the school bus that drives glucose into every cell in your body. So, not enough insulin in your blood means there are not enough school buses driving our glucose children into the cell. Not enough glucose inside the cell means we have the beginning of a very serious situation.
TYPE 1 - PANCREAS UNDER ATTACK
Let's jump back to type-1 for a moment. The numbers show that type-1 diabetes makes up about 10% of all diabetes cases and typically affects children under age 18. It can, however, affect adults as well - Mary Tyler Moore developed type-1 diabetes in her 30's after beginning the Mary Tyler Moor Show in the early 1970's. What makes type-1 diabetes unique is that it is an autoimmune disorder in which the immune system malfunctions and mistakenly attacks the insulin making beta-cells in your pancreas. Diagnosis of type-1 diabetes is confirmed by measuring a person's blood for specific antibodies known to attack the pancreas and can be confirmed by determining insulin output through a test known as the C-peptide test. Remember, type-1 diabetes means the person is not producing enough insulin in their pancreas - and with too little insulin our glucose friends will not be able to get into the cell to keep it working properly.
ANSWER IN FRONT OF US THE ENTIRE TIME
What is very exciting about type-1 diabetes is that scientists believe there is potential for significant reversal if the source of the autoimmune disorder can be removed. What we're talking about is not from some investor driven promise of a new pancreas or some other elaborate device, but instead, suggests the cure for this disease may very well have been in front of us all along. In a statement by researchers at UCLA David Geffen School of Medicine, they stated and I quote,
"Most people with long-standing type-1 diabetes have beta-cells that continue to be destroyed. The mechanisms underlying increased beta cell death may involve both ongoing autoimmunity and glucose toxicity. The presence of beta-cells despite ongoing apoptosis implies, by definition, that concomitant new beta cell formation must be occurring, even after long-standing type-1 diabetes. We conclude that type-1 diabetes may be reversed by targeted inhibition of beta cell destruction.
In other words, they are saying that if we can get rid of the autoimmunity causing beta-cell destruction, the beta-cells should be able to grow back and provide the body with sufficient insulin without the need for external shots. As you'll read shortly, scientists from major research centers around the world have identified dozens of common chemicals in our lives that cause autoimmunity and beta-cell destruction. Since these are now facts and no longer "theories" - it strongly suggests of something people with diabetes can do to reverse their illness.
WHAT'S A PANCREAS?
Your pancreas is located next to your liver and stomach. While its main job is to make enzymes to digest food, about 2% of your pancreas contains small round structures called islets (pronounced i-LETS). On average, the pancreas has about 2 million islets that appear like tiny round islands under a microscope. Within the boundaries of each islet are about 1000 beta-cells whose job it is to make insulin and release it into your blood at just the right time. Taken altogether, this works out to about 2 billion beta-cells in your pancreas (if your lucky).
NOT ALL PANCREAS' ARE CREATED EQUAL
As seen in upcoming research, autopsies of children who died in accidents other than related to diabetes show something interesting and worrisome. Some children are born with far fewer islets than others. In fact, in a study of dozens of deceased children, some had less than 500,000 islets while others of the same age had several million. Why this great variation? No one has the answer just yet, but we need to find out very soon as having low numbers of islets and beta-cells at birth would predispose anyone to type-1 diabetes at a much younger age.
TYPE 2 - YOUR CELLS ARE PROTESTING
The cousin to type-1 diabetes is type-2. Type-2 diabetes is not an autoimmune disease in which insulin making beta-cells in the pancreas are under attack. Instead, the cells throughout your entire body and brain are the source of the problem, however this time, there is plenty of insulin and glucose, but for some reason (which researchers have yet to identify), your cells won't let enough of the insulin/glucose buses inside. Unlike type-1, with type-2 diabetes, the pancreas is still able to make sufficient insulin, so you would think they would welcome the insulin/glucose bus with open arms, but they don't. So basically, your cells are involved in some kind of a protest and begin blocking the entry of some of the insulin buses. In other words, cells in the body and brain are "resisting" the entry of the insulin and glucose and why the term "insulin resistance" is often used in describing diabetes. While scientists understand why type-1 diabetes occurs, as of 2017, they still did not understand why insulin resistance occurs with type-2 diabetes.
INSULIN AND GLUCOSE PARTY IN THE CELL
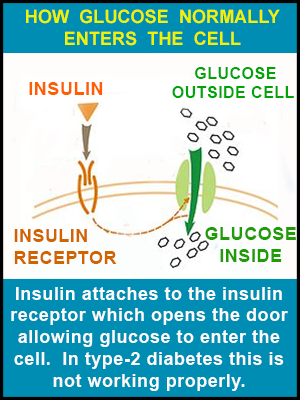 Before letting you go, let me explain this in a way that will paint a picture for better understanding type-2 diabetes. The cells in your body are basically a round spherical shape. Coated along the cell surface are a number of doors - some are marked "INSULIN" and others "GLUCOSE." Your beta-cells in your pancreas produce insulin which enters the blood traveling to all different parts of your body. When Mr. Insulin comes to his door - the door-keeper immediately recognizes Mr. Insulin and let's him inside. Once inside, the door-keeper yells to his friend guarding the glucose door and says, "Mr. Insulin is here, you can now let in Mrs. Glucose." The glucose doors open and Mrs. Glucose (being the life of the party she is), gets everybody in a great mood and things are wonderful! The problem with type-2 diabetes appears to lie with the door-keepers as they don't always recognize and allow Mr. Insulin through the door and into the cell. Maybe some kind of grudge from a previous party, but the bottom line is the door-keeper (officially the insulin receptor) resists letting Mr. Insulin inside so he is left out in the cold - and if Mr. Insulin can't get in his door then Mrs. Glucose can't get in her door either. For those wishing to research this further, the scientific term for the insulin door is the insulin receptor and for glucose it is the glucose transporter. Type 2 diabetes is responsible for about 90% of all diabetes cases and typically raises its ugly self in older individuals, although since the 1990's, it has been occurring at higher and higher rates in children 10-18 years old.
Before letting you go, let me explain this in a way that will paint a picture for better understanding type-2 diabetes. The cells in your body are basically a round spherical shape. Coated along the cell surface are a number of doors - some are marked "INSULIN" and others "GLUCOSE." Your beta-cells in your pancreas produce insulin which enters the blood traveling to all different parts of your body. When Mr. Insulin comes to his door - the door-keeper immediately recognizes Mr. Insulin and let's him inside. Once inside, the door-keeper yells to his friend guarding the glucose door and says, "Mr. Insulin is here, you can now let in Mrs. Glucose." The glucose doors open and Mrs. Glucose (being the life of the party she is), gets everybody in a great mood and things are wonderful! The problem with type-2 diabetes appears to lie with the door-keepers as they don't always recognize and allow Mr. Insulin through the door and into the cell. Maybe some kind of grudge from a previous party, but the bottom line is the door-keeper (officially the insulin receptor) resists letting Mr. Insulin inside so he is left out in the cold - and if Mr. Insulin can't get in his door then Mrs. Glucose can't get in her door either. For those wishing to research this further, the scientific term for the insulin door is the insulin receptor and for glucose it is the glucose transporter. Type 2 diabetes is responsible for about 90% of all diabetes cases and typically raises its ugly self in older individuals, although since the 1990's, it has been occurring at higher and higher rates in children 10-18 years old.
NUMBERS ARE MORE THAN SHOCKING
The statistics you're about to read on diabetes rates vary as different agencies report different numbers - so explanations will be included. However, the latest figures available show that over 14% of the adult U.S. population has diabetes when counting people with doctor diagnosed diabetes and those with undiagnosed diabetes. Undiagnosed simply means the person has diabetes, as measured by a fasting blood sugar over 125, but didn't know it. The chart above is from the CDC website - it doesn't show the 14% number just mentioned because it includes children and represents only doctor diagnosed diabetes, but does give a excellent visual of the diabetes increase over the past 50 years. As seen from the chart, the percentage of all people in the U.S. with diagnosed diabetes has been rapidly increasing - going from less than 1% in 1960 to over 7% in 2014. As you'll soon read, this rapid rise cannot be explained by an aging population or growing rates of obesity - and is certainly being caused by something else. As mentioned, this 7% number is actually lower than the true diabetes rates, as 5% of adults today have diabetes and simply don't know it. So, to give a clearer picture on this - the CDC did another study but this time included those with undiagnosed diabetes in their 2014 National Diabetes Statistics Report. Instead of 7%, they now show that 9.3% of people of all ages in the U.S. have either diagnosed or undiagnosed diabetes. It's also important to note that children rarely get diabetes. Numbers from 2012 in the same CDC report state that children under 18 account for only one-quarter of 1% of all diabetes cases, although child diabetes is now increasing faster than adult diabetes and will be discussed later.
DIABETES RATES IN ADULTS
To get a picture of diabetes rates in just adults, the same CDC report also gave numbers for only people 20 years and older. This time, the diabetes rate increased again and showed that 12% of adults age 20 and older had either diagnosed or undiagnosed diabetes. (Again, these numbers were calculated using 2012 figures so are most likely considerably higher today).
Other studies show higher diabetes rates for adults. As described by Dr. Any Menke in the September 8th issue of the Journal of the American Medical Association, a detailed analysis of 2,781 adults from the National Health and Nutrition Examination Survey from 2011 to 2012 showed a diabetes rate of 9.1% for doctor diagnosed cases among all races and a 14.3% diabetes rate when including both diagnosed and undiagnosed. So whether it's 12% or 14%, the diabetes epidemic is not increasing solely because of an aging population - if it was, we would only see increases in people over age 60, but we are not. Diabetes rates are increasing in people in all age groups and in both people of excess and normal weight. When looking at the chart above, the rates for diabetes doubled on average every 20 years from 1960 to 2000, but now, when also taking into account undiagnosed diabetes, it looks as if diabetes is doubling every 15-20 years and possibly less. As you can see, diabetes in the U.S. is now a train headed down a mountain with no brakes and gaining speed.
OLDEST ADULTS HAVE LOWER DIABETES RATES
While it is true that diabetes rates are considerably higher when looking at people over age 60, something very interesting apears when separating this group further and looking at diabetes rates people even older. For some unexplained reason, diabetes rates for people born before World War II have a lower diabetes rate than those born after the war. For example, as reported in the 2011 Annals of Saudi Medicine, people over age 70 had a diabetes rate of 64%, however, people who were 10-20 years younger had a 69% rate of diabetes. Why older people born before WWII have a 5 percentage point lower rate of diabetes is certainly a mystery, and certainly takes the steam out of any argument that diabetes is increasing simply because people are getting older. If aging was the major reason, we simply wouldn't see older people born before World War II with lower rates of diabetes. This detectable pattern will most likely fade as those born before 1945 pass-away, thereby elimininating this important evidence, however, it needs to be remembered as one more piece of critical evidence presented to the jury.
PREDIABETES: A CRYSTAL BALL TO YOUR FUTURE
OK, so let's look at these numbers again. It appears that adults 20 years and older have a diabetes rate of around 12-14%. Now, let's discuss more on the topic of prediabetes that was briefly touched upon earlier. Like a crystal ball into your future, prediadiabetes can predict with fairly good accuracy when you will get diabetes and is another reason why you need to find out yesterday if you have prediabetes. Once you know you have it, there is now a lot you can do to stop the train in its tracks - improve your blood sugar scores and dramatically delay the onset of diabetes and possibly prevent it altogether. This will also be explained shortly.
DIFFERENCE IN DIABETES AND PREDIABETES
While 14% of us reading this most likely have diabetes - how many of us have prediabetes? While full-diabetes is defined as having a morning fasting blood sugar level of 126 or higher (which you can measure with a one minute $15 test from Walmart), prediabetes is defined as having a morning fasting blood sugar a little lower from 100 to 125. The latest numbers from the American Diabetes Association (published in the journal Lancet) show that when testing blood samples from the adult U.S. population - 38% of us have a fasting blood sugar of 100 to 125 - in otherwords - 38% of us had prediabetes in 2012. The next common sense question - What actually happens inside our bodies that makes us go from healthy - to prediabetes - to full diabetes? Regarding type 1 diabetes, it's just simple math. Autopsy studies of people dying within one year of a type-1 diabetes diagnosis show that 70-90% of their beta-cells in the pancreas have been destroyed. But what about people with prediabetes - do they show damage to their pancreas? In similar autopsy studies, if you have prediabetes (a sugar level between 100 and 125), the pancreas' of these people show a 40-60% loss of beta-cells. This is valuable information as there now appears to be much you can do to delay and prevent full diabetes
IF THIS DOESN'T SCARE YOU...
While 38% of us in 2012 had prediabetes, what is extremely concerning about this number is that the same American Diabetes Association study found that 75% of people with prediabetes will in fact develop full-blown diabetes within 10 years. So, let's do the math - 75% of the 38% with prediabetes equals about 25%. Therefore, those of us with prediabetes right now will add another 25 percentage point increase to the current 14% diabetes rate over the next 10 years. Adding these two numbers together gives a total of 39%. Even if 1/4 of the original 14% with diabetes die within 10 years, we will still have over 35% of the U.S. population with full-blown diabetes by 2022. This represents an astounding increase to say the least. Imagine for a moment if 35% of the adult U.S. population has diabetes in 2022 (along with the increased rate of child diabetes), the personal and financial consequences upon society will be horrific. On January 1, 2017, the manufacturer of the diabetic insulin known as Lantis increased its price by 60%. I imagine this will also not be their last increase before 2022 for this expanding and lucrative disease.
TYPE-1 DIABETES IN CHILDREN
Our previous numbers have focused on rates for both type-1 and type-2 diabetes combined among all ages and for adults. To get a handle on just the rates of type-1 diabetes in children, researchers at the National Publich Health Institute in Finland began a global investigation of 27 countries and published their findings in the 1999 journal Diabetologia. For children under age 15, they determined that type-1 diabetes increased on average 3% per year from 1960 to 1996, resulting in a yearly incidence rate of about 15 new cases of type-1 diabetes per 100,000 people. The authors also predicted (back in 1998), that new cases of type-1 diabetes would rise to 30 per 100,000 per year for children worldwide by 2010. Congratulations to the authors - their prediction was quite accurate. In the United States, the CDC reported in their 2014 National Diabetes Statistics Report (pg. 4) that type-1 diabetes was about 29 per 100,000 for non-Hispanic white children ages 0 to 9 and about the same rate for children age 10 to 19.
YOUNGEST CHILDREN HAVE HIGHEST DIABETES INCREASE
An even more worrisome pattern was seen when investigating type-1 diabetes among children of pre-school age and younger. As reported in the September 1997 British Medical Journal, diabetes rates more than tripled for children under age 5 in the Oxford region of the United Kingdome during the 11 years from 1985 to 1996. In 1985 there were about 4 new cases of diabetes per year for these children, however, by 1996, there were nearly 18 new cases of diabetes per year for the same age group. This works out to a doubling of type-1 diabetes among our youngest of children every 4-5 years and is an absolutely shocking increase. Also of interest, this same rapid increase among our littlest children in the UK was also seen in the United States. Certainly, as many scientists agree, there is something in and around us that must be driving this exponential growth in diabetes and is certainly beyond anything than can be explained by genetics or obesity.
AGE DIFFERENCES IN DIABETES
To add more clarity to the numbers, let's now look at total diabetes (diagnosed and undiagnosed) for different age groups from numbers the CDC derived from 2011-2012 statistics and published in their 2014 Report. At this time, they reported that diabetes rates for children under 18 was only 1/4 of 1%. For people age 20-44, diabetes rates were 5%. For those age 45-64, diabetes was 17.5% and for those over 65 diabetes was affecting 33% of the group. This report did not give numbers for people over age 75 separately (which in other studies shows lower diabetes rates). For those of you who like tables we can show it this way.
RACIAL DIFFERENCES IN DIABETES
Another fact that raises a lot of questions is why diabetes rates differ so dramatically among races? When breaking down the numbers, the 2014 CDC Report stated that while whites have an adult diabetes rate of about 10% - blacks and Hispanics have an adult diabetes rates more than double this at over 20% (2012 figures). If trends continue with a doubling of diabetes every 12-20 years (since 2012), the African American and Hispanic populations will have a whopping 40% diabetes rate sometime between 2012 and 2020 and possibly sooner - with whites reaching that number 10-20 years after that. The fact that African American and Hispanic populations have higher rates of diabetes is a fascinating observation and studies show this may not be coincidence. Interestingly, in several studies discussed on the following pages, African Americans and Hispanics have far higher levels than whites of a chemical class known as "thallates" (actually spelled "phthalates." In fact, in a large study of African Americans discussed shortyly, they were found to have nearly twice the blood levels of this chemical than whites, and interestingly, have twice the level of diabetes than whites. Higher levels of phthalates has been shown in many different studies to be associated with higher rates of diabetes. Some cultural practices also suggest a potential for higher use of the chemical as it is typically used as a thickening agent in plug-in air fresheners, perfumes, colognes and in a variety of cosmetics and skin lotions for dry skin.
When looking at racial differences in this 2011 study, total diabetes (a fasting blood sugar 125 or higher) was 11% for whites - 20% for Asians - 22% for African American - and 23% for Hispanics. Hispanics and African Americans have similar diabetes rates in most studies and typically twice the rates of whites. Again, these figures were from 2011-2012 so they are most likely considerably higher today (2017). As shown below, treating diabetes is quite expensive due to daily insulin shots resulting in costs of about $1000 per month for every person with diabetes. Any way you look at it - if 30-40% of the adult population has diabetes in the next 10 - 15 - 20 years then each of us will be paying an additional $200-$300 out of pocket each month to care for adults and children with diabetes. Personally, I'd like to put that money somewhere else - for example, using it for replacing the causes of diabetes - which can be done. The obstacle here being that many companies make considerable profits from the compounds being linked with diabetes so letting go won't be easy. Obviously, no one can afford increases in insurance premiums of this amount to pay for diabetes and this literally has the potential to bankrupt our medical insurance system and decimate the quality of life for the vast majority in Americans.
PREDICTIONS DRAMATICALLY WRONG
BY WORLD HEALTH ORGANIZATION (WHO)
I wasn't sure whether to laugh or cry when looking at future predictions of diabetes by government agencies. The Centers for Disease Control (CDC) and World Health Organization (WHO) typically look at past trends of an illness to predict future rates. This is helpful in making sure financial and medical resources will be in place when needed. Well, the WHO did this in 1998 and the CDC did this in 2001, and to say their predictions were wrong is an understatement of many magnitudes and would be laughable if not for the severe consequences all of us will soon face. Here is a direct quote from the scientists involved in the WHO report published in 1998, from the journal Diabetes Care, Volume 21, page 1414.
Prevalence of diabetes in adults worldwide
was estimated to be 4.0% in 1995
and to rise to 5.4% by the year 2025.
Think about this - the WHO predicted in 1995 that 5.4% of the world would have diabetes by 2025 (which includes both diagnosed and undiagnosed diabetes and only for people above age 20) - So, just how far off were they? Now, that we are 20 years into the future let's go to the WHO website and see how accurate they were. In the Diabetes section of their website under "Key Facts" - under the "Media Centre" tab they state the following:
The global prevalence of diabetes
among adults over 18 years of age
has risen from 4.7% in 1980 to 8.5% in 2014.
So, to review one more time - the World Health Organization kept the calm by predicting in 1995 that the world would have a diabetes rate of only 5.4% by the year 2025. But here, on their website today, they state that in 2014 the world was showing an 8.5% rate of diabetes. In other words, the rate of diabetes is each year is not advancing at a steady peace like they thought - instead, the percent of any population with diabetes is continuing to rise faster each year after year after year. While the World Health Organization predicted our planet would have a 5.4% diabetes rate in 2025, we actually hit 5.4% around 2005 - some 20 years ahead of schedule - and that should make your hair stand on end.
What's very interesting is that diabetes rates differ dramatically from one country to the next. For example, some impoverished countries in Africa have a diabetes rate of under 1% while Saudi Arabia has one of the highest adult diabetes rates in the world clocking in at over 30% - and that was back in 2010. What risk factors do they have in Saudi Arabia that poor areas of Africa with 1% diabetes rates don't? Well, along with the hundreds of oil wells and chemical refineries dotting the horizon and spewing toxic gasses into the air, when we investigated further we found what could be one of their biggest contributors. Unlike most developed countries that dispose of trash in landfills, the Saudi's have opted instead for inexpensively burning trash at ground level. In the United States this is illegal because burning household trash in open areas creates the chemical dioxin at very high levels - one of the most potent diabetes inducing chemicals on the planet. Unlike other chemicals that break down over time- dioxin builds up in the body and fat tissues and wreaks havoc on the immune system at infintesimal levels of parts per trilliion. When trash containing either plastic - chlorinated white paper or colored paper is burned at low temperatures in land fills (or backyard barrels) - it forms very high levels of dioxin, that rains down on those unfortunate neighborhoods downwind from the source. Children who play outside on the ground then ingest additional amounts through finger mouth touching etc.
Getting back to the WHO report and to make sure we truly compare apples with apples, we do know that diabetes in the U.S. was about 14% for diagnosed and undiagnosed for people above age 20 in 2012. This means the U.S. rates were more than double the WHO's 2025 prediction 11 years before 2025!
CDC DIABETES PREDICTION EVEN FURTHER OFF THE MARK
The World Health Organization is not alone, the Centers for Disease Control (which represents only numbers in the United States), did their own diabetes prediction study, but this time they made a prediction for rates for the year 2050 instead of 2025. Here is a direct quote from the scientists involved in the CDC report published in the 2001 journal Diabetes Care, Volume 249, pg 1936.
The number of Americans with diagnosed diabetes
is projected to increase 165%,
from 11 million in 2000 (prevalence of 4.0%)
So, using their best statisticians and researchers, the CDC told us back in 2001 that we could expect to see about 7% of the population with diabetes by the year 2050. Let me say this again, the CDC predicted back in 2001, as published in the journal Diabetes Care, that by the year 2050, the U.S. population will most likely have a diabaetes rate of 7%. Well, to be courteous, let's just say they were a little off... Ah, heck with being courteous - these guys were light years off target! Now that we are 15 years in the future we can do a little fact checking - In looking at the latest CDC chart of diagnosed diabetes of all ages, we can in fact see that diabetes won't hit 7% in 2050 - and that's because it hit 7% in 2014 - 36 years ahead of schedule! In fact, if counting those with undiagnosed diabetes, and looking at the trends mathematically, the U.S will most likely have a diabetes rate of at least 50% or higher by 2050 - not the 7% predicted by the 2001 CDC Report.
WHY IS DIABETES INCREASING?
When my son was 12 years old he became very ill in May of 2016. He was vomiting continuously and no one knew why. Unfortunately, I left for Florida two days before he became ill so I wasn't able to monitor his condition. When he did become ill his mother recommended he drink ginger-ale as she believed this would help reduce his vomiting. No discredit to her as ginger-ale is the typical and recommended treatment for nausea. Our son ended up drinking nearly an entire liter and by now he was extremely sick and vomiting even more. At this point, his mother came home from work and took him to the doctor. Eventually, the doctor gave him a blood sugar test and it was 550. Translation? He had diabetes as normal blood sugar should be around 100. So, back to the question - why is diabetes increasing so rapidly today in developed countries? Now, someone may also make the case that we are getting better in diagnosing diabetes and that is why the numbers are going up. However, unlike other illnesses, type-1 diabetes usually comes in like a lion as a person with type-1 diabetes often develops a condition known as ketoacidosis. This is a fancy term meaning their little bodies can't properly use glucose for energy so it begins burning fat and muscle for energy instead (nature's back-up mechanism), resulting in a trip to the ER and immediate and obvious diagnosis. Another argument is that diabetes is increasing because our population has increased and we simply have more people in the older age groups. While this does increase the number of people with diabetes, it would not increase the percent of people with diabetes (unless diabetes was actually becoming worse). Since the percent of people with diabetes is in fact increasing each year in all age groups (including children), it clearly shows that an increased older population is not the primary reason and something else must be happening.
THE OBESITY SMOKE SCREEN
Being overweight is a risk factor for diabetes - you've heard that before right? The person is overweight because they eat too much - so it's their fault they got diabetes. Simple answer, sounds good - case closed. Not so fast.... While it is true that obese people do have higher rates of diabetes, if you think about it, this actually proves nothing. In fact, here's another risk factor for diabetes - being a white normal weight child under age 5. For some unexplained reason, type-1 diabetes has grown faster among young white children than any other age or racial group. This is a statistical fact reported in the CDC Report and being overweight has absolutely no relationship to type-1 diabetes. While our ancestors have been walking this planet for over 5 million years - what are the odds that obesity and diabetes both begin increasing at dramatic rates and at exactly the same point in time in our existence? A one in a billion coincidence to say the least.
CHEMICALS LINKED TO DIABETES ALSO INCREASE OBESITY
When you get to the meat and potatoes of this report, you'll read summaries from dozens of peer reviewed medical journals from major universities and research centers showing increased rates of diabetes for people exposed to pesticides - car exhaust - chemicals in cosmetics - disinfectants - fragrances, as well as a number of chemical food additives and more.
For example, The addition of these chemicals to consumer products increased dramatically after World War II and gives more of a clue as to why younger people born before WWII have higher rates of diabetes than older people born before the war. While investigating the connection between obesity and diabetes, a fascinating pattern appears: Many of the same chemicals being linked with diabetes are also being found to increase obesity. This is very important so I"ll state this again; Many of the same chemicals in consumer products that scientists are finding can alter glucose metabolism and increase diabetes are also being found to affect weight and increase obesity. For example, in a collaborative study done between the University of Minnesota and Kyungpook National University in Korea, researchers studied over 2,000 people and found that those with the highest levels of 6 specific chemicals (all used in homes and consumer products) had a diabetes rate over 35 times higher than people who had the lowest levels of these chemicals. While this alone is an absolutely unprecedented increase, what makes this even more interesting is that these 6 chemicals are also in a class of chemicals known as endocrine disruptors. This is important for you to understand so don't fall asleep on me just yet. You need to know that the endocrine system consists of glands like the ovaries, thyroid, adrenal gland and the pancreas. This cute little parts of the human body secrete hormones which then travel through the blood to tell other organs to do something - and this "something" is usually quite important. The problem is, just as the name implies, endocrine disrupting chemicals have been found to copy (or mimic) natural hormones in the body which fools the body think that these synthetic chemicals are hormones being secreted by other parts of the body - when in fact, they are not. As you can imagin, this hormone confusing situation could cause serious problems for the human body. Some of our hormones play a critical role in in regulating body weight and fat deposition (not to mention blood sugar levels ) so you can imagine the biological chaos that is occuring if we are routinely exposed to endocrine disrupting chemicals. You've most likely heard stories from friends or neighbors in which someone took a certain medication and immediately gained weight - they weren't eating more, but for some reason, taking a certain pill for some ailment or condition resulted in dramatic weight gain. This is accepted knowledge in medical practice and is listed as a side effect on many drug labels. This gives a classic quick example of how a petroleum based chemical taken at a specific time can function as an endocrine disruptor and alter weight. In fact, when people with obesity are studied specifically, there are consistently found to have higher levels of these endocrine disrupting chemicals in their bodies - and this now appears not be coincidence.
OBESITY INCREASING IN ANIMALS & PETS
This one may give yo a chuckley, but obesity isn't just happening at higher rates in humans, what's very interesting is that it is also happening to animals as well. In a study published in the November, 2010 Proceedings of the Royal Society, researchers found that weights of all types of animals has increased with each passing decade over the past 20-40 years. For example, their study of 574 cats found that between 1990 and 2002, female cats experienced a 13.6% increase in obesity with each decade along with a 5.7% increase in body weight per decade. Similar increases were seen in horses and many other types of animals. In conclusion, the scientists stated the following as a potential explanation,
One set of putative contributors to the human obesity epidemic
is the collection of endocrine-disrupting chemicals (endocrine-disruptors),
widely present in the environment.
WHICH CAME FIRST...
THE OBESITY CHICKEN OR THE DIABETES EGG?
While we're constantly reminded that obesity is a "risk factor" for diabetes, we could just as well say that diabetes is a risk factor for obesity. In fact, looking at the numbers, our medical history books show us that increasing rates of diabetes really started taking off in the 1930's, 40's and 50's. It would be interesting to investigate this further to see if childhood weight gains occurred before or after the increases in diabetes. Even for those still holding onto the simplistic explanation that obesity is the reason for diabetes, it still doesn't explain the even faster increase in type-1 diabetes among children of normal weight. While diabetes is stated to be increasing about 2-3% per year for all age groups, it is growing at over 5% per year for children under age 5. Certainly, this points us in the direction that something is happening during pregnancy and/or right after birth that weakens or damages the mechanisms in the body that control normal blood sugar and prevent diabetes.
In a study that dramatizes this situation, researchers at UCLA David Geffen School of Medicine received permission from the Mayo Clinic to examine the pancreas' of 46 children who died suddenly and did not have diabetes. They counted the number of what is called islets (pronounced i-lets) in the pancreas' of these children. If you remember from your previous 30 second biology lesson, islets make up about 2% of the pancreas and are round island shaped structures that contain the beta-cells which produce insulin. As you well know - not being able to produce enough insulin is what causes type-1 diabetes.
Results from these deceased children show a wide variation in their number of islets, ranging from about 400,000 in some children to over 4 million in others (study details below). Since type-1 diabetes occurs over many years as islets are slowly destroyed by a malfunctioning immune system, being born with a lower number of islets (and beta-cells) would certainly predispose that child to developing diabetes at a much younger age. However, two questions remain - What circumstances can damage or slow islet growth in pregnancy and what environmental circumstances are able to damage the remaining islets once a child is born?
FINANCIAL COSTS UNSUSTAINABLE
FOR DIABETES IN 10, 15, 20 YEARS
Since diabetes rates are increasing dramatically, it makes sense to do a study on the costs of diabetes. Such a study was done and published in the September 2014 journal Diabetes Care. One of their main findings - the cost for taking care of someone with diabetes was about $11,000 per year in 2014. This covers such things as daily insulin, needles and doctors visits. The report went on to say that the economic burden associated with diabetes - prediabetes - and diabetes in pregnancy exceeded $322 billion in 2012, consisting of $244 billion in excess medical costs and $78 billion in reduced productivity. What's important to understand (and helpful for predicting the future), this 2012 cost is nearly 50% higher than the $218 billion cost from diabetes just 5 years earlier in 2007.
When looking at the cost per person, treating someone with diabetes in 2012 averaged $10,970 per year, $5,800 for diabetes in pregnancy and $4,030 for undiagnosed diabetes and $510 for prediabetes. Payments to doctors and drug companies treating those with diabetes comes primarily from Medicare and insurance premiums. The report stated that each person in the U.S. (including those who don't have diabetes) is paying an additional $1,000 per year out of pocket to cover the medical expenses for people with diabetes. In other words, if rates of diabetes were the same as back in the 1950's and 60s, your insurance premiums would be on average about $1000 less per year - or looking at this another way, your employer could be paying you an additional $1000 per year if diabetes rates were the same as 50 years ago. Unfortunately, diabetes rates in 2014 were about 15 times higher than in the 1950's and 60's and continues to grow.
THIS IS WHERE IT GETS SCARY
While the cost of treating someone with diabetes is expensive - at about $12,000 per year - if it was only for 1% of the population (as in 1960), then costs are spread out through the population as a whole and not that significant. However, diabetes rates are no longer at 1% and have now increased to about 10% in 2014 for all ages if including undiagnosed diabetes, and about 14% for those more than 20 years old. So, this is where it gets scary - if diabetes rates will in fact double over the next 15 years (as suggested by looking at rates and expected growth of prediabetes) then by the year 2022, 30-35% of the U.S. population over age 20 will have diabetes (double this for blacks and Hispanics). So, if you and I were paying $1000 per year out of pocket in 2014 for people with diabetes - then by the mid 2020's, we will each be paying closer to $2000 per year and with medical inflation, probably closer to $3000 per year. Folks! that's 200-300 bucks out of your pocket every month just to care for this one illness. This doesn't even take into account that people with diabetes then develop other illnesses at higher rates as they get older, thereby compounding the problem even further.
DIABETES IN CHILDREN GROWING EVEN FASTER
There were approximately 500,000 children under age 15 with type-1 diabetes in the world in 2013 (Diabetes Research Clin Pract). In the U.S., looking at people under age 20, there were an estimated 18,436 people younger than age 20 with newly diagnosed type-1 diabetes in 2008-2009 and 5,089 people under age 20 with newly diagnosed type 2 diabetes. Compared to other racial groups, white children had the highest rate of new cases for type-1 diabetes (CDC Report pg.3). In a study done by the University of Colorado and reported in the journal Diabetes Care, type-1 diabetes was increasing about 2.7% per year for children aged 0 to 17 between two measurement periods from 1978-88 and 2002-04. Researchers found that incidence rates for diabetes went from about 15 per 100,000 children in 1978-88 to approximately 24 per 100,000 children in 2002-2004. This represents a dramatic 60% increase in about 15 years. Rates of new diabetes cases for people 20 years or older were much higher at 780 per 100,000 (see report from CDC pg.3 top). Rates are increasing even more rapidly in China, where pollution and parent exposure to chemicals is far worse than in the U.S. For example, between 1997 and 2011, in China's largest city of Shanghai, type-1 diabetes was doubling every 5-7 years with an annual incidence increase of 14% per year ( World J Pediatrics)
AN ILLNESS CAUSED BY THE ENVIRONMENT
Diabetes is the poster child for an illness caused by chemicals used in modern society. For a quick background - type-1 diabetes is the most common form in children. It occurs when insulin making beta-cells in the pancreas are attacked by a malfunctioning immune system. In fact, all children under age 10 with type-1 diabetes are found to have autoantibodies in their blood that attack the pancreas. This renegade immune system doesn't happen normally, it can only happen if the thymus gland is not filtering out autoimmune cells (as it normally does) and also if your natural killer cells lose their ability to remove autoimmune cells (Natural killer cells are also part of the immune system and work as a back up mechanism for removing autoimmune cells when the thymus is unable to do so). These two critical autoimmune protecting and anti-diabetes systems have been shown to weaken after exposure to a myriad of chemicals from plastics to disinfectants - to pesticides - to car exhaust. Yes, even the automobile is under attack for worsening diabetes over the decades. For example, as reported in the May 2015 issue of Environmental Health, diabetes rates were 30% higher for people living less than 330 feet from high traffic roadways (who breathe higher levels of gasoline engine exhaust chemicals).
Another environmental source strongly linked to diabetes comes from people who spray mosquito contorl pesticides. In a study done at Aarhus University in Denmark. Diabetes was more than 11 times higher among workers who spray mosquito control pesticides than others of the same age and weight not spraying the chemicals.
A 2012 Harvard Medical School study showed that African American women with the highest levels of the cosmetic chemical called phthalates (pronounced "thallates") had twice the rate of diabetes as women with the lowest levels of phthalates. Interestingly, African American women in general have about 90% more phthalates in their blood than whites and may be due to cultural habits of lotions containing phthalates and increased use of fragrances. Another study investigating phthalates was done in Sweden among 1,016 elderly patients aged 70. Results showed that those with higher levels of the phthalate known as MiBP had lower insulin secretion and patients with higher levels of phthalates known as MEP and MMP had increased problems with insulin resistance.
YOUR HOUSE AS THE CAUSE OF DIABETES
This next study will make you want to pack your bags if you live in an older home. Researchers from four separate colleges from around the world followed 90 healthy non-diabetic young adults for 23 years. The results were reported in the journal Diabetes Care and found that people whose bodies had higher levels of the banned pesticide chlordane and chemical known PCB had what is called reduced insulin sensitivity. This means their bodies were not using insulin properly and is what the culprit in type 2 diabetes. Both chlordane and PCB's are found in the indoor air of older homes because of their common use before the 1980's. PCB's were used in caulking and varnishes of older homes and chlordane was the termite pesticide of choice during that era. It is also formed as an unintentional by-product during the chemical formulation of house paints today and is was found to be at highest levels in yellow paints.
TIME TO PANIC
Regarding the CDC's dramatically wrong estimate discussed earlier on diabetes predictions for 2050, it may not have been 100% their fault. While one can argue they may have done this intentionally to avoid "panic" over increasing diabetes rates, their predictions may have been so far off because back then they believed that diabetes rates were increasing through what is called a linear trend. This simply means that when drawn on a line graph, the line continues in the same direction and at the same angle. Unfortunately, this is not the case as more recent line graphs show a dramatic steepening of the line which is known as an exponential increase. In other words, things are getting a lot worse and in a lot less time. Translation? It's time to panic...... Also, for some reason there is a large delay in government agencies reporting more recent diabetes rates. We don't need numbers from 7-10 years ago, we need them from last year so we can truly see how fast this is increasing. We also need the government to report not just diagnosed diabetes but also include figures with undiagnosed diabetes and keep up to date prediabetes numbers as well.
WHY YOU SHOULD BE SCARED AS HELL
ABOUT GETTING DIABETES - THE HEALTH CONSEQUENCES
First, once you get diabetes or even prediabetes, your days of binging on popcorn, cookies or ice cream during your favorite TV show or movie will be history - nada - gone - done. While abstaining from these bits of fun can make life only marginally worth living, it's the least of your worries. To make sure the glucose floating in your blood can get into your cells and provide them with energy, you'll become an insulin junkie and will be giving yourself shots several times a day. To make sure you don't overdose on insulin (which could kill you in an hour), you'll be using scales and measuring cups to portion your food to make sure you eat just the right amount of carbohydrates for each shot. Once you get accustomed to becoming a human pin cushion, you can start pondering what other health surprises loom in the distance - and sorry to say - there are many. Your first surprise is that you'll be in the morgue sooner than your friends without diabetes - in fact, you'll be lying there about 12 years sooner. So, what's going to put you there? Apparently you are going down sooner from a combination of increased autoimmune attacks on healthy tissue and the higher blood sugar spikes that typically occur with diabetes. The following is a direct quote from page 5 of CDC pamphlet on diabetes.
Diabetes can affect many parts of the body
and is associated with serious complications,
such as heart disease and stroke, blindness,
kidney failure, and lower-limb amputation
Upon investigating health problems linked with diabetes from the National Library of Medicine, we found that the CDC left out a few other important health problems from diabetes. For starters, your likelihood of getting cancer goes way up. In a study that was ironically conducted by the Center for Disease Control - they found your chance of colorectal cancer was 30% higher if you have diabetes. Being that booty cancer is common among men already, a 30% increase is not good news. But hold on, you have more to look forward to; In a study sponsored by the National Institutes of Health, men with diabetes had a 4 times greater risk of developing liver cancer and women had double the risk. In this same study kidney cancer was 40% higher in men and 70% higher for diabetic women. Pancreatic cancer is one of the deadliest of all cancers with most people dying within the first year of diagnosis. It happens to about 1.5% of the U.S. population, but if you have diabetes, your odds have increased to to about 3% for this painful and quick killing disease.
Let's now take a look at one of the most common cancers for women. Breast cancer wil develop in about 1 in 8 women at some point in their lives. If you are a woman with diabetes your odds are even worse - Australian researchers reported in the journal from the Society of Endocrinology that results from 59 separate studies on breast cancer found that diabetes increases the risk of getting breast cancer by about 20%. So, instead of a 1 in 8 chance you now have closer to a 1 in 6 chance of getting breast cancer.
But we're just getting started - cancer is not the only disease that increases if you have diabetes. Your chances of adopting a white cane to find your way around the house is much higher as well. Yes, wer're talking blindness. In fact, the most frequent cause of new cases of blindness for adults aged 20-74 years is from a disease called retinopathy. Retinopathy is when the blood vessels inside your eye are slowly destroyed. Eye doctors can see the damage when looking into your eye during an examination. During the first two decades of having diabetes, nearly all patients with type-1 diabetes have retinopathy and more than 60% of people with type 2 diabetes show signs. People with retinopathy have been found to have immune system antibodies that mistakenly attack the retina - just as people with type-1 diabetes have immune system antibodies that attack the pancreas. All of this provides evidence that diabetes is just the first illness to crop-up from a body being destroyed by the immune system.
The most recent 2014 CDC pamphlet on diabetes (page 6) states the following statistics on increased health problems once you get diabetes. First, your chance of having a heart attack is 80% higher than people of the same age without diabetes. Kidney failure is also much higher with 44% of all new cases of kidney failure coming from people with diabetes. Blood pressure is higher as well - 71% of people with diabetes have blood pressure greater than 140/90 or used medications to lower blood pressure. Having a stroke was 50% more likely for adults with diabetes. Outcomes after having a stroke was also worse for diabetics as reported in the 2000 journal Diabetes Care. Of 229 nursing home patients in Barcelona who had a stroke, 26% of those without diabetes died. For those unlucky ones with diabetes, 54% died after the stroke. Bottom line - once you get diabetes, not only does your life expectancy instantly drop 12 years, but the remaining years of your life will be now be associated with many more health problems than people without diabetes - unless you can persuade your immune system to give up its self-destructing behavior.
GIVE YOURSELF THE TEST FOR GOD'S SAKE
Since diabetes is turning into an epidemic with potentially devasting consequences for society - everyone should be tested at least twice a year for diabetes and prediabetes. In fact, with the new studies that have come out over the past 10 years, the information from this simple test can literally tell you how much of your pancreas is damaged and give you a much needed warning of upcoming prediabetes and diabetes! The test is simple to do and takes only a minute. It can even be done at home without going to the doctor's office if so inclined. It is called a glucose test and costs $10-$15 from the pharmacy department at Walmart, Krogers or practically any drug or grocery store. They usually keep it right on the shelf in the diabetes section. Test kits range in price greatly but most stores have the generic cheaper ones that can be 75% less. Some test kits don't contain the test strips so you may have to buy those separately (read the label). So, after shelling out the 10 or 15 bucks for the test kit and strips, take it home and read the instructions so you can become friends. When you wake up the next morning simply prick your finger before breakfast with a nearly painless device included in the kit - and put the small drop of blood from your finger onto the test strip in the meter. After 5 seconds you'll see a number and hopefully it will be around 80 as it is for most people. Apparentlhy, people with numbers around 75 have a very healthy pancreas, but most people today test in the low 80's so that's a good target number for starting. If your number is from 90 to 99, your pancreas may be sending up its first signal flare that a little rebellion is going on. If it is between 100 and 125 you have what is called prediabetes and your pancreas has possibly lost an estimated 30-40% of its beta-cells (this occurs with type-1 diabetes but odds are you have type 2 or a combination of the type1 and type2 if over age 20. Mary Tyler Moore developed type-1 diabetes in her 30's).
As mentioned earlier, the American Diabetes Association states that 75% of people with morning blood sugar numbers between 100 and 125 develop full-blown diabetes within 10 years.
What is very interesting now is that studies clearly show without any doubt whatsover - humans do in fact have the ability to regenerate lost or damaged beta-cells, and apparently a lot more than previously thought. Regeneration has been found to occur from several places inside the human body including special areas in the pancreas known progenitor ducts - and also from the simple division of beta cells themselves. Along with this, new beta-cells have also been shown to from from the altruistic sacrifice of alpha-cells. You can't help but love these guys - alpha cells apparently really care about their beta-cell brothers. They make up about 20% of the cells in the islets and work to do the opposite of what beta-cells do. Instead of lowering blood sugar as insulin does, if blood sugar gets too low, they release a hormone called glucagon. This tells the liver to open the gates and release some of its stored glucose. So, if your alpha cells are working good, you won't get low bood sugar. What is so exciting is that alpha-cells can magically transform into a beta-cell when needed. That's what I call a friend.
Scientists have found that type-1 diabetes will come to you much faster if you get high blood sugar levels since this in itself has been shown to damage or weaken the remaining beta-cells you have. You should be able to see where this is going. Since high sugar levels can accelerate damage to your pancreas, it is certainly helpful to know if you have prediabetes (and risk for higher sugar levels) since you can then actively avoid those ice-cream and cookie binges and prevent this destructive process. In fact, keeping blood sugar levels low suggests that this may in fact accelerate the ability of the pancreas to grow new beta-cells.
OVERWHELMING RESEARCH
LINKING ENVIRONMENT TO DIABETES
In the research studies outlined next, you'll see studies done by major universities across the world linking diabetes with many environmental circumstances including chemicals in cosmetics, plastic packaging in food, perfumes, air fresheners, plastic water bottles, dish washing soaps, chemicals in polyester clothes, chemicals in nail polish, detergents, common pesticides purchased from grocery stores, gasoline fumes during your next fill-up as well as breathing car exhaust itself (to name just a few). As you recall, if you are going to develop type-1 diabetes, don't worry, you need to lose 70-90% of your beta-cells in your pancreas before problems appear - right now you are most likely only at 20 or 30% damage so you have a little time. If you have prediabetes - studies suggest you are at about 40-60% damage, but at least if you know that, there is now a lot you can do.
WE REALLY ARE RUNNING OUT OF TIME
It is currently January of 2017 at the time of this writing and the most recent number we have for diabetes is 14% from 2012. We hear reports that global warming will cause dire consequences in 100 years - but with diabetes on track to hit 50% of the U.S. population in 15, 20 or 30 years and with African Americans and Hispanics hitting that number in 10-20 years - global warming may be the least of our worries. It is noteworthy to mention that generating concern about diabetes should be much easier than with other health and environmental issues because it has the potential to cause severe health problem among so many people right now and in the very near future - even those in politics who often appear conscience challenged should be more willing to take notice because it could affect them at any moment. Unlike most other serious diseases, once identified, prediabetes can be slowed, and possibly reversed by eliminating exposure to the now dozens of identified environmental sources along with preventing glucose beta-cell damage now shown to occur from higher sugar levels. This will lead to lower autoimmunity and increased growth of new beta-cells (which has been shown to occur in both animals and humans). Also, by bringing attention to the environmental causes of diabetes, we are simultaneously addressing many other health problems linked to the same environmental sources. For example, while living close to highways and breathing car exhaust has been linked to increases in diabetes, it also has been linked with increases of child asthma, autism, Alzheimer's and cancer. Along with these increasing health problems, many chemicals linked to diabetes are the same ones that contribute to global warming. For example, car exhaust again. By converting our vehicles to run off natural gas immediately (which can be done for the cost of about one or two months of diabetic supplies)), rates of diabetes would drop quickly along with the carbon that accelerates global warming. So the next time you get a chance, spend a few bucks on an inexpensive glucose test meter from your store of choosing and find out if you have prediabetes with numbers from 100-125 or if you are closer or better than the national average of around 82. Seven months ago my morning blood sugar numbers were averaging in the prediabetes range of around 110 - today they are closer to 95. Unfortunately, my 13 year old son was diagnosed with type-1 diabetes in May of 2016, but thanks to him, I've been able to learn about this disease and push back my diabetes clock by many years.
Researchers Believe
Increase of Type-1 Diabetes is from Environment
Dr. Fredrick Miller is director of the Environmental Autoimmunity Group at the National Institute of Environmental Health Sciences in Bethesday MD. In talking about diabetes and other autoimmune illnesses, Dr. Miller stated in the June 2011 issue of Environmental Health Perspectives,
Our gene sequences aren’t changing fast enough to account for the increases (in diabetes),” Miller says. “Yet our environment is—we’ve got 80,000 chemicals approved for use in commerce, but we know very little about their immune effects...
Dr. Miller oversees research investigating environmental factors associated with autoimmune disorders. In this report, Dr. Miller also discussed research on identical twins in which one twin often develops autoimmune disorders and the other does not, thereby providing further evidence that diabetes is a result of environmental factors and not genetics.
In another report, published in the 2002 December issue of Diabetes, Professor Edwin Gale also agrees that the environment is the main reason for the diabetes increase.
A rapid change in incidence within a genetically stable population implies that nongenetic factors are active and that the influence of genes is relative to population, time, and place. It suggests that something has changed in the environment our children encounter or in the way they are reared.
3 Autoantibodies
as Primary Cause of Type-1 Diabetes
Autoantibodies are antibodies in the blood that have malfunctioned for some reason. Normally, antibodies attack foreign invaders such as bacteria or viruses. However, in type-1 diabetes, B lymphoctye white blood cells malfunction and produce antibodies against healthy insulin producting beta-cells of the pancreas. When autoantibodies attach to the beta cell, they act like magnets and attract other immune system white blood cells which then destroy the beta cell. This increased destruction of beta-cells continues for years until about 80% of beta-cells are destroyed, thereby resuting in diabetes (NOTE: New studies suggest that this is much less and closer to 50% at diagnosis.) The three primary autoantibodies identified that destroy beta-cells in the pancreas include:
GADA
Glutamic Acid Decarboxylase Autoantibody |
The GADA antibody attacks the GAD65 enzyme in beta-cells in the pancreas. GAD65 produces GABA which is involved in regulating insulin output. |
IA-2
Islet Antigen-2 Autoantibody |
IA-2 is a major target for islet cell autoantibodies. The protein is found in up to 80% of children and adolescents with T1 diabetes. |
IAA
Insulin AutoAntibodies |
IAA's are autoantibodies that target insulin itself. They were present in 18% of 112 newly diagnosed type-1 diabetics prior to beginning insulin treatment. See 2nd journal listing in SCIENCE.
|
Quote from researchers in the study: "... the current tests for autoantibodies to these three autoantigens are highly predictive of type-1 diabetes.
DIABETES
Vol. 54 (suppl 2.S52), Dec. 2005
Dr. Catherine Pihoker
Dept. of Pediatrics & Medicine
University of Washington
Seattle, Washington
SCIENCE
Insulin Antibodies
Dr. JP Palmer et. al
Vol. 222(4630): 1337-1339, Dec. 1983
1 of 5 Siblings of Diabetic Child
have Autoantibodies
Having 2 Antibodies = 90% Chance of
Future Diabetes
If your brother or sister has type-1 diabetes - you have about a 20% chance of having autoantibodies as well - that's one of the conclusions of this study conducted by the Diabetes Research Center in Finland. Since typically all children who develop type-1 have autoantibodies attacking their pancreas - having an accurate way to measure and predict future diabetes in siblings would be extremely helpful to doctors and families. Like a window to the future, this is now being accomplished by identification of different types of autoantibodies in childrens' blood. As discussed previously, type-1 diabetes occurs when the immune system malfunctions and mistakenly destroys beta-cells through different processes including making antibodies against the pancreas. In this study, researchers wanted to investigate if autoantibodies against the pancreas were higher in brothers and sisters of diabetic children, and therefore, help in predicting future diabetes. To answer this - 180 non-diabetic siblings of diabetic children were tested for four different autoantibodies. Children were all under age 6 at the time of testing. Antibodies tested included islet cell antibodies (ICA), glutamate decarboxylase antibodies (GADA), insulin autoantibodies (IAA), and antibodies called islet antigen-2 (IA-2A). After adding up the numbers, they found that nearly 20%of all siblings had one or more autoantibodies against their pancreas beta-cells. Breaking this down to individual antibodies, they found that 12% of the 180 children had islet cell antibodies - 7% had insulin antibodies - 8% had GADA antibodies, and about 8% were positive for the IA-2A antibodies. The next important thing to find out was how many different types of antibodies a child had, as having more than one antibody type greatly increases the risk of sooner appearance of diabetes. So, when looking further into the numbers - they found that 16 of the 180 children (about 9%) had one detectable antibody - 5 (about 3%) had 2 antibodies and another 12 children (7%) had 3 or more antibodies. These cooperative 180 children were then followed over the years until they reached age 10 to see how many developed diabetes. Results showed that 15 of the 180 children (18.3%) developed clinical type-1 diabetes sometime before age of 10. What's noteworthy about this, the ones who developed diabetes were the ones who typically had more than one of these renegade antibodies. For example, of the 15 children who developed diabetes, 13 of them were in the group that had 2 or more antibodies. Looking at this in another way - of the 17 children who tested positive for 2 or more autoantibodies - 15 of them (nearly 90%) developed diabetes before age 10. In other words, if your child had 2 or more pancreas autoantibodies, they had a 90% chance of developing diabetes within about 5-7 years. Whether this percentage holds true for larger groups of children remains to be seen, but a number of studies are underway to find this out conclusively. One thing that can be taken from all of this is that autoantibodies play a significant part in taking the pancreas beta-cells out of action, but it also exposes a fascinating silver lining; If we can identify situations in our environment that cause autoantibodies to form, and we remove these "situations," we potentially set up the scenario where we can either delay the onset of diabetes or possibly even allow the pancreas to regenerate once the antibodies are no longer present and destruction is stopped, thereby significantly delaying and possibly even preventing the disease. In conclusion, the researchers stated,
These observations suggest that disease-associated autoantibodies can well be used as surrogate markers of clinical type-1 diabetes in primary prevention trials targeting young subjects with increased genetic disease susceptibility.
Body's Autoimmune Filter (Thymus)
Weakened by Pyrethroid Pesticide
Your thymus is arguably the most important part of your body for preventing every autoimmune disease - including diabetes. While originally thought to be important only in childhood and adolescence, the thymus has now been shown to play a crucial role in adults as well. Located in the central upper chest, your thymus functions as a "maturing and growth area" for many important immune system cells that attack viruses and cancer - but this is just the beginning, more recently, the thymus has been found to act as a "filter" - with the ability to remove millions of autoimmune cells from the body. Like a policeman giving a sobriety test to a drunk driver, your thymus literally tests immune system cells for their ability to identify self and non-self. If immune cells are smart and can recognize the difference between good cells (self) and bad (nonself such as viruses) - they are allowed back into the bloodstream highway. If the immune cell fails the test, such as identifying healthy body cells as invaders, they are destroyed on the spot. This critical role clearly shows that any environmental circumstance that can damage or weaken the thymus police could potentially lead to a massive increase of damaging autoimmune cells entering the bloodstream - resulting in severe negative health consequences (such as type-1 diabetes).
In this study, researchers at the Dept. of Environmental Toxicology at University of California wanted to find out if the common pyrethroid pesticide deltamethrin could damage the thymus in live animals. Deltamethrin is popular among pest control operators in the U.S. and is used in home pest control, agriculture and golf-courses. Animals were given a single injection of the pesticide at doses ranging from a low of 6 mg/kg to 50 mg/kg. The thymus was then removed from the animals after 24 hours and examined. Even at the lowest dose at 6 mg/kg - resulted in the thymus losing 22% of its weight after 24 hours with increased reductions in weight as dosages increased. The researchers then performed another test to see how time affected the thymus after pesticide exposure. After exposing animals to 25 mg/kg of deltamethrin for 24 hours, the thymus weight was reduced by about 41%. During the next two weeks, the thymus continued to shrink in size daily reaching a maximum 50% reduction in weight after 2 weeks. For a bit of good news - the thymus also demonstrated the ability to regenerate as it steadily regained about 1/3 of its weight after 35 days at which point the study was ended. In conclusion, the researchers said the reduction of weight to the thymus was due to the thymus cells being destroyed by the pesticide through a process known as apoptosis. While the thymus was in a steady pace of increasing weight when the study ended at 35 days, it is not known how much more the thymus would have regenerated after 2 months, 3 months, etc. This study further increases encouragement for potential reversal of diabetes as the organ that protects us from type-1 diabetes does show signficant potential to improve function, but only when circumstances shown to cause damage are removed.
Biochemical Pharmacology
Abstract -
Full Text PDF
Vol 51: 447-454, 1996
Dept. of Environmental Toxicology
Intitute of Toxicology and Env Health
Center for Environmental Health Sciences
University of Califiornia
Davis, CA, USA
Autoimmunity Starts Here
Damage to the Thymus Gland
Like deltamethrin, permethrin is also a pyrethroid pesticide commonly used in mosquito control - agriculture - and indoor and garden pest control. It is also used as a topical skin treatment for preventing insect and mosquito bites. In the second study listed at right, researchers applied a single topical dose of the pesticide permethrin to the shaved skins of 5 week old mice in gradually increasing doses. As found with deltamethrin in the study above, permethrin also showed the ability to decrease the number of thymus cells - with 52% destruction of the thymus from 15 microl of the permethrin and 80% thymic destruction from 25 microl of permethrin. This major destruction to the thymus occurred after just a single permethrin skin application. In a real life situation - children often receive permethrin applications many times a week and in some cases daily.
International Journal of Toxicology
Vol. 19(6), 383-389, Nov 2000
Food Chemical Toxicology
Vol. 40(12): 1863-73, Dec 2002
This Part of Beta Cell Involved
in Insulin Release - GAD65 & GABA
As mentioned above, GAD65 is an enzyme in beta-cells that produces the compound known as GABA. Increased levels of GABA then result in increased insulin secretion by beta-cells.
QUOTE FROM STUDY AUTHORS: ... autocrine GABA, via activation of GABAARs, depolarizes the pancreatic β-cells and enhances insulin secretion. On the other hand, insulin down-regulates GABA-GABAAR signaling presenting a feedback mechanism for fine-tuning β-cell secretion.
Public Library of Science
October 21, 2011
Dr. Paul Bansal, et al.
Departments of Physiology & Medicine
University of Toronto, Canada
Acceleration of Type-1 Diabetes
if IA-2 Autoantibodies Present
IA-2 is a beta-cell damaging antibody known as the insulinoma-associated protein-2. The function of the protein remains unclear but appears to be involved in enhancing insulin secretion. The frequency of IA-2 is similar in the USA and Europe and ranges between 60-80% in newly diagnosed type-1 diabetic patients. Children positive for IA-2 autoantibodies have accelerated progression of type-1 Diabetes.
Autoantibody Levels Lower After 12 Years
Scientists at Lund University in Sweden wanted to determine if there was a relationship between beta cell function and levels of autoantibodies in diabetic patients at diagnosis and then 12 years after diagnosis. The study was conducted with 107 adult diabeteic patients between the ages of 21 and 73. Results showed complete beta-cell failure (as measured by C-peptide testing) occurred only in patients who had islet antibodies at diagnosis. This included 77% of patients with multiple antibodies (16 of 21) and 80% of those with GADA antibodies (4 of 5). Interestingly, while most GADA positive patients still remained GADA positive after 12 years, patients with two or three antibodies at diagnosis had significantly lower levels of antibodies after 12 years. In keeping with this, the percentage of patients positive for all 3 islet autoantibodies decreased from 37% of patients at diagnosis to only 15% after 12 years. Among patients with two or three islet antibodies at diagnosis, complete beta-cell failure (undetectable fasting P-C-peptide) was present in 74% of patients (20 of 27) after 5 years
DIABETES -
FULL TEXT
Vol. 51(6): 1754-62, June 2002
Department of Endocrinology
Lund University
Malmo University Hospital
Malmo, Sweden
Test Determines Insulin in Blood -
Identifies Type-1 or 2 Diabetes
Also Measures if Diabetes
is Worsening or Improving
It has typically been reported that 80-90% of all beta-cells in the pancreas are damaged at the time of type-1 diabetes diagnosis. However, this number has been challenged with new autopsy studies published in 2017 found this number is actually closer to 50% in type 1 diabetes (depending on age). Whether it is 90% or 50%, the remaining beta-cells still have the ability to produce some insulin. Insulin output can be measured in patients through a blood test known as C-peptide. When beta-cels are in the process of making insulin, C-peptide is produced as a by-product. Therefore, the amount of C-peptide in the blood can be used to accurately determine the amount of insulin being made by beta-cells. The C-peptide test can also be used to help determine if the patient has type-1 or type-2 diabetes as patients with higher C-peptide would be more likely to have type-2 diabetes. Patients with type-1 diabetes can also be given the C-peptide test yearly to determine if their beta-cells have stopped producing insulin or have improved insulin production (via regeneration of pancreas or reduction of autoantibodies). Rather than measure direct insulin in the blood, it is preferable to measure C-peptide as it does not get metabolized by the liver (which does occur with insulin) Depending on the measurement criteria, normal reference ranges for C-peptide are 0.8 - 3.1 ng/ml or 0.26-1.03 nmol/L.
WebMD
C-Peptide Blood Test
Type 2 Diabetes Being Redefined
as Autoimmune Disease
While type-1 diabetes is an autoimmune disease in which the immune system mistakenly destroys the pancreas, type-2 diabetes has long been considered only a metabolic disorder - having nothing to do with autoimmunity. However, evidence now shows this is no longer the case. In new research from Stanford University School of Medicine, type-2 diabetes is also being shown to be an autoimmune disorder. In one part of the study, lead author Dr. Shawn Winer, found that immune system T-cells and B-cells begin attacking healthy tissue in mice when their fat cells grow too quickly. When the scientists used mice that lacked these B-cells, the obese mice did not develop insulin resistance. The scientists then carried this research to humans. Here they studied 32 age and weight matched overweight people who differed only in their sensitivity to insulin. When comparing the two people in each group of same weight (one with insulin resistance and the other without) the researchers stated, "We were able to show that people with insulin resistance make antibodies to a select group of their own proteins. In contrast, equally overweight people who are not insulin-resistant do not express these antibodies. Dr. Winer, then went on to state,
It's highly suggestive that your body targets its own proteins as part of the develoment of insulin resistance. It really links the concept of insulin resistance with autoimmunity.
New Beta-Cells Grow in Pancreas
by Division of Older Beta-Cells
In principle, new beta-cells can grow from stem cells (as occurs in blood, skin and intestine) or by duplication of existing cells. Giving a brief review of previous studies, the researchers stated new beta-cells are believed to grow from cells lining the pancreatic ducts - from inside the islets - or in bone marrow. Like catepillars to butterflies, other studies suggest that new beta-cells form in adults when cells called acinar cells located in the islets transform into beta-cells. In this current study at Harvard University, researchers found a way to show that the major source of new beta-cells formed in adults (and in pancreas damaged in mice) is from pre-existing beta-cells, rather than stem cells.
CHEM-TOX COMMENT: If this study is correct (that new beta-cells form from existing beta-cells), it suggests the importance of removing autoimmune factors before total destruction of all beta-cells in the pancreas.
NATURE
Vol. 429: 41-46, May 2004
Dept. of Molecular and Cellular Biology
Howard Hughes Medical Institute
Harvard University
Cambridge, Massachusetts
Yuval Dor, et. al
A Healing Pancreas?
Diabetic Patient Achieves Nomal Insulin Output Years after Diagnosis
The following provides an example of one patient with GADA autoantibodies at diagnosis who on further testing 12 years later no longer had the antibody and who also had normal insulin production. Again referring to the original study above of 107 adults diagnosed with diabetes, patients were tested in follow-ups at 3, 5 and 12 years after the orignal diagnosis of diabetes. Follow-up testing showed nearly all patients had worse (lower) insulin output (as measured by the C-peptide test) as years progressed. Complete beta-cell failure was present in only 4 of the 107 at diagnosis but was present in 21 patients five years later. It is interesting to mention that while insulin output decreased for nearly all patients during the 12 years, several patients did not follow the trend and were actually found to produce normal levels of insulin 5 and 12 years after diagnosis. More precisely, of the 5 patients positive for GADA antibodies at time of diagnosis, 4 of these individuals developed complete beta-cell failure after 12 years, however, the 5th patient did not. In fact, the 5th patient showed significantly improved insulin output from his beta-cells. Three years after diagnosis, his C-peptide levels were 0.55 nmol/l - however, 5 years after diagnosis, he no longer had the GADA antibodies and C-peptide had increased to 1.09. After 12 years his C-Peptide levels were still in the normal range at 1.08 nmol/l.
DIABETES -
FULL TEXT
Vol. 51(6): 1754-62, June 2002
Department of Endocrinology
Lund University
Malmo University Hospital
Malmo, Sweden
View reference to patient with improved insulin output in "RESULTS" section under heading
"Patients with one antibody at diagnosis" - second paragraph.
Prison Inmate Experiences
Fascinating Remission of Diabetes
Doctors report an very interesting case where a 32 year old female experienced complete remission of type-1 diabetes. The woman was admitted with symptoms of blurred vision and general stomach and chest pain. Her initial workup showed a random blood glucose of 938 mg/dl, an A1C of 12.7% and a +2 on the urine ketones dipstick test. Her GAD antibody assay was 0.09 (normal is ›= 0.02 nmol/L). Her C-peptide level (used to determine insulin output) was 0.70 ng/ml (normal is 0.78 to 5.19 ng/mL). For her treatment she was on basal bolus insulin for the first 4 months after diagnosis. The patient was then sent to prison for unknown reasons and was unable to take any insulin while in prison. Interestingly, she had no symptoms of hyperglycemia or ketoacidosis while in prison. After 7 months she was released and contacted her doctors. At her medical follow-up immediately after being released (and not taking any insulin for 7 months), her A1C was 5.6% and fasting blood glucose was 98 mg/dl. She did have an unintentional weight gain of 14 pounds since the orignal diagnosis. Currently (14 months after her diagnosis), she is still in complete remission, not requiring insulin therapy.
CHEM-TOX COMMENT: This demonstrates another case in which someone with severe type-1 diabetes (A1C of 12.7%) was basically "cured" of their condition. It is interesting to note that the remission occurred after being removed from her normal surroundings and being placed into a new environment and after not receiving insulin
19 Year Old Young Man
Experiences Remission of Type-1 Diabetes
Another case of diabetes remission occurred in this 19 year old patient who entered the hospital with ketoacidosis, a fasting blood sugar of 432 mg/dl and an A1C of 12.3%. He was also positive for the beta-cell attacking autoantibodies called GAD (glutamic acid decarboxylase) which were measured at 46 units/ml. He began an intensive program of both insulin glargine and insulin glulisine at the prescribed dose of 0.5 units per kg body weight. After one month, the young man began to show lower glucose levels so doctors began reducing his daily insulin injections. This pattern continued and by 8 weeks he no longer needed insulin and entered complete remission with fasting glucose of between 70 and 130 and an A1C of 7.8%. At a one year follow-up, he was still in complete remission with an A1C of 5.8% and fasting glucose of 108 mg/dl. His fasting C-peptide was 1 ng/ml and a 75 gram glucose test was 152 mg/dl after 2 hours with a C-peptide of 4.3 ng/ml. After 15 months taking the drug sitagliptin only, he had an A1C of 6.3% and fasitng glucose of 122 mg/dl. GAD antibodies were still positive at 6 units/ml.
9 Year Old Boy Off Insulin
after Beginning Paleolithic Ketogenic Diet
 In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
The diet was introduced gradually over a 5 day period. During this time insulin was adjusted according to fingerstick glucose measurements and beginning on the 6th day (February 18, 2014) the child was on the full Paleolithic ketogenic diet. To measure insulin output, doctors performed the C-peptide test again with results of 1.1 ng/ml. This is within the normal range of 0.9 - 7.1 ng/ml. Since glucose was normal before and after meals, the doctors stopped his daily insulin injections. Not only did this child have much more stabilized blood sugar levels but also experienced complete elimination of low blood sugar which was frequent while on insulin. After being on his new diet for 19 months his A1C levels were between 5.2 and 5.6%.
Int J of Case Reports & Images
Vol. 6(12): 752-757, 2015
Evolutionary Medicine Working Group
Budapest, Hungary
Dept. of Neurology
University of Pecs, Hungary
Honeymoon - Partial Remission:
What is this Exactly?
Parents often hear doctors refer to something called the "honeymoon period" after a child has been diagnosed with type-1 diabetes. This is a patient-friendly term that means the person is showing signs of improved pancreas insulin output and therefore less of a need for external insulin shots. Not all children are lucky enough to achieve a "honeymoon." Numbers from different studies show only about 50-70% of children diagnosed with type-1 diabetes bounce into the honeymoon, with the higher percentage going with older children and lower percentage for children under age 5. The honeymoon period usually begins one month after diagnosis and peaks at 3 months. It is believed to occur because of improved new growth of beta-cells within the child's pancreas. It then begins a gradual decline over the year. Apparently, different doctors use different criteria to define the honeymoon period. Using the latest definition of the honeymoon period (called insulin dose-adjusted A1C), about 60% of children are in the honeymoon 3 months after diagnosis - 50% at 6 months - and only about 25% of patients are honeymooning at 12 months. The term partial-remission is also used to describe the honeymoon period, therefore, both terms refer to the same observation. Some facilities describe the honeymoon (or partial remission) as having an A1C of 7.5% or less while others define it as an A1C of 6% or lower. For those not familiar with diabetes, the A1C (same as HbA1C) is considered a more accurate way to measure blood glucose. This number is used to give us more of an average blood glucose level over the past 6-8 weeks, rather than just one day. Six to eight weeks is the lifespan of a red blood cell and red blood cells are like a sponge which gradually soak up glucose during this time. Another definition used to describe the honeymoon period is when the child has a daily insulin dose in units that is less than half their weight in kilograms. For us Americans, that means hitting the internet to first convert pounds into kilograms. For example, a 120 lb child has a weight of about 54 kilograms. If the child is taking less than 27 units daily (27 is half of 54), then he/she could be considered in partial remission (or experiencing a honeymoon). One of the newest definitions of partial remission (and takes a little more time to calculate) was proposed by Dr. Henrik B. Mortensen at the Glostrup University Hospital in Denmark. Their method is called IDAA1C which stands for insulin dose-adjusted A1C. This is a mathematical formula that first calculates the daily dose of insulin in units per kilogram for the child and multiplies this by 4, and then adding this to the child's A1C%. Yes, I know I lost you on that, but here's an example to make it easier to undersand. My son has a weight of 124 lbs which is about 56 kilograms. He takes about 12 units of insulin daily including his nightime Lantis. Bringing out the calculator, we are going to divide 12 by 56. So, we type in 12, press the divide symbol and then hit 56. This gives us the decimal 0.47. Next, we multipy .47 x 4 and get 1.8. The final step is to add this 1.8 to his last A1C of 5.5 which gives us a score of 7.3. Since anything less than 9 is considered partial remission, we can say that my son Alan is still in his honeymoon (or partial remission) after having diabetes for 8 months. This latest definition for partial remission is a little more difficult to achieve but is said to be more accurate at predicting actual insulin production. How long does the honeymoon last? Only 25% of those who reached the honeymoon at all are still there after 12 months, which works out to about 15% of all people diagnosed with type-1 diabetes. So, if your child makes it to 12 months and still is in partial-remission you are doing something right so congratulations!
Diabetes Care
Vol. 32(8): 1384-1390, Aug 2009
Glostrup University Hospital, Denmark
Dept of Pediatrics, Hannover, Germany
University of Ulm, Germany
University Children's Hospital, Switzerland
How Often Children Achieve Remission
and Partial Remission
of Type-1 Diabetes
To determine if and how often remission and partial remission occurred in children, researchers in Kuwait studied 103 recently diagnosed diabeteic children under the age of 12 and followed their conditions for several years.
Of the 103 diabetic children unger than 12 years old, partial remission occurred in 71 children and complete remission in 3. Remission tyipically begain about 29 days after diagnosis and continued for an average of 7 months. All children had lost their remission status after 13 months with most ending after 7 months. The honeymoon perdiod was defined as having insulin requirements of less than 0.5 Units per kilogram body weight per day and an A1C of less or equal to 6%.
Pediatric Diabetes
Vol. 7(2): 101-107, April 2006
Endocrine Unit, Pediatric Dep
Farwaniya Hosspital, Kuwait
Remission & Partial Remission
in 242 Diabetic Children
What to expect when your child gets diabetes is the question burning on the mind of every parent. Parents wonder if their child will have it for life? - Are some cured of the disease? - What health consequences to expect, etc. In this study out of Belgiu - 242 children under age 15 were followed after diagnosis of type 1 diabetes. Blood tests were taken at 1 month, 6 months and 12 months to look for changes in glucose and insulin output to see how their conditions progressed. While no children achieved complete remission (where no insulin was needed), 56% of the group did achieve the definition of partial remission (also called the honeymoon period) which lasted 9.2 months on average after diagnosis. Partial remission was defined as having an A1C below 6%.
Blood samples also showed a steady decline at each testing period. No children were shown to have improvement of insulin output during the 12 months.
High Blood Sugar Can Worsen
or Cause Diabetes
by Damaging
Beta-Cells in Pancreas
We're all guilty of this one... Sometimes we go overboard and eat a lot more carbs and sugar than we should. For the men reading this, think of that time you got dumped by your girlfriend of 2 months. In the subsequent days (or minutes) after rejection, you may have chosen to down a gallon of Bryer's Vanilla along with a six-pack of those chocolate Doodles. Over the next hour, unbeknowingst to you, your blood sugar went from 100 to 150 to 200 and up past 250. After flying in the stratosphere for 30-45 minutes, your pancreas finally regains consciousness and brings you back down to 130. While you may have noticed nothing in your time of turmoil, this most likely wasn't an event without consequences. Scientists are finding out that situations such as this can in fact be quite harmful to the beta-cells and cause what is called "Glucose Toxicity." This is actually what preceded my 12 year old son's diagnosis of diabetes while he drank a liter of Ginger Ale over a few hour period in hopes of alleviating nausea he was experiencing
In a study from the first study from the University of Washington Pacific Northwest Research Institute, scientists found that high levels of glucose in the blood can weaken and damage genes involved in insulin production. Since genes are the brains that control everything going on in the cell - this is certainly not a good thing - just like losing a girlfriend.
In another study from the University of Washington, scientists this time wanted to know if beta-cell insulin output was hurt more by short term high exposure to glucose or by moderate glucose levels over a longer period of time. To figure out this one, insulin producing beta-cells were cultured in test tubes containing different levels of glucose. First, they confirmed that higher glucose resulted in lower insulin output, but then if they were exposed to lower than normal levels of glucose, they showed a dramatic improvement in insulin output.
There are currently high profile medical websites stating unequivocally that there is nothing we can do to prevent type-1 diabetes, however, this study clearly shows that is not the case. In fact, if someone knows they have prediabetes (or getting close to it), that they can in fact do quite a bit to slow the development of the disease by simply making sure they buy only single serve ice cream instead of those gallon sizes when their relationship is a bit shakey.
Researchers state "Type 1 Can Be Reversed"
Evidence of New Beta Cell Growth
in People with Type-1 Diabetes
Insulin secretion is detectable in some people with long-standing type-1 diabetes, indicating either a small population of surviving beta-cells or continued renewal of beta-cells subject to ongoing autoimmune destruction. In this study, 42 individuals with type-1 diabetes and 14 non-diabeteic individuals were evaluated for presence of beta-cells, beta cell apoptosis (destruction), beta cell replication and T-lymphocytes and macrophages. Results showed 88% of people with type-1 diabetes had active living beta-cells. Beta cell destruction was twice as likely in type-1 diabetes as control subjects. In conclulsion, the researchers stated,
Most people with long-standing type-1 diabetes have beta-cells that continue to be destroyed. The mechanisms underlying increased beta cell death may involve both ongoing autoimmunity and glucose toxicity. The presence of beta-cells despite ongoing apoptosis implies, by definition, that concomitant new beta cell formation must be occurring, even after long-standing type-1 diabetes. We conclude that type-1 diabetes may be reversed by targeted inhibition of beta cell destruction.
Diabtologia
Vol. 48(11):2221-8, October 5, 2005
Larry Hillblom Islet Research Center
UCLA David Gefen School of Medicine
Los Angeles, California
Diabetes Higher in Women
Exposed to Cosmetic Chemical
Researchers at Harvard Medical School studied levels of a common cosmetic chemical in 2,350 women between the ages 20 and 79. The chemical, called phthalates (pronounced thallates), is used in most personal care products such as perfumes, body lotions, facial skin creams and also in plug-in air fresheners. These chemicals have been banned or restricted in Europe, but as of 2017, they were still being used in the U.S. In their opening sentence, the researchers stated, "previous studies have shown women have higher urinary concentrations of several phthalate metabolites than do men, possibly because of a higher use of personal care products."
To determine if this chemical was linked to causing diabetes, researchers compared the levels of phthalates in women with diabetes with those without diabetes. Results showed that women who had the highest 25% levels of the chemical had almost twice the rate of diabetes as women whose phthalate levels were in the lowest 25% group. It is also important to note that some of the phthalates were associated with insulin resistance among women who did not report a diagnosis of diabetes. Because insulin resistance often precedes type 2 diabetes, this finding suggests that some phthalates may affect type 2 diabetes risk by effects on insulin resistance. In addition, the authors stated they found other phthalate metabolites to be associated with an increased odds of diabetes, as well as fasting blood glucose levels and insulin resistance. Two additional points of interest were found in the study: Women with a larger waist circumference (more than 94.5 cm) had higher overall phthalate levels as women with a smaller waist circumference), thereby suggesting the chemical may increase the risk of obesity. Also, African Americans had about 90% higher levels of phthalates in their blood as whites. In conclusion the researchers stated,
These findings suggest that other phthalates might affect type 2 diabetes risk either through glucose dysregulation or insulin resistance. If future studies determine causal links between phthalates and diabetes, then reducing phthalate exposure could decrease the risk of diabetes among women.
Chemical Used in Fragrances & Cosmetics
Causes Autoimmunity
Type-1 diabetes is an autoimmune disorder in which the immune system attacks the pancreas. The chemical phthalate (pronounced "thallate") is widely used in plastics, children's toys, polyester clothes and cosmetics (including perfumes, air-fresheners, skin creams and cosmetics). Scientists report here that exposure of mice to phthalates results in the formation of anti-self DNA antibodies. Phthalates are a class of chemicals known as benzene dicarboxylates. In conclusion, the scientists said their study was the first to demonstrate that exposure to phthalates results in production of autoreactive B-Cells.
Immunology
Vol. 103(4): 482-492, December 2003
Dr. So-Yon Lim & Swapan K Ghosh
Dept of Life Sciences
Indiana State University
Terre Haute, Indiana, USA
Fasting Blood Glucose Worsens by 6 Points
from Fragrance Chemical
The chemical called phthalates (pronounced "thallates") is used as a thickener and solvent in most fragrances including perfumes, colognes and typical plug-in air fresheners. Researchers in this study wanted to investigate if phthalate levels in the blood could affect fasting blood glucose levels. To determine this, investigators from Harvard Medical School took blood samples from 3,083 non-diabetic individuals age 12 to 79 and measured for levels of phthalates. Results were then divided into four equal groups (quartiles) from lowest to highest levels of phthalates. This was done for non-Hispanic whites, non-Hispanic blacks and Mexican-Americans. Scientists then compared the fasting blood glucose levels for those in the lowest 25% phthalate group with those in the highest 25% phthalate group. Results showed that for whites, people in the lowest phthalate group had about 2 points lower fasting blood glucose than those in the highest 25% phthalate group. Results for non-Hispanic blacks showed those in the lowest level phthalate group had about 3.5 points improved fasting blood glucose levels than those in the highest phthalate group. Mexican-Americans had the most dramatic difference showing those in the lowest phthalate group had a fasting blood glucose that was 5.8 points lower than those in the highest phthalate group.
CHEM-TOX COMMENT: Because of cultural practices, Mexicans and African Americans typically use more phthalates than whites. In one study, blacks were found to have a 90% higher level of phthalates than whites in general. This may be because of increased use of not only fragrances, but also lotions used for dry skin (which also contain phthalates). Also, Tthe differences in this study is only for quartiles. among quartiles. It would have been more beneficial to see how rates changed if divided into 5% or 10% groups for potentially identifying even greater differences. For example, whites having phthalate levels equal to that found in the highest Mexican-American quartile may have showed the same improvement, but because of cultural practices.
Enivronmental Health
Vol. 13(1): 6, Feb 2014
Dept of Medicine
Brigham & Women's Hospital
Harvard Medical School, USA
More Cosmetics & Plastics = Fatter Waistline
Also Increase Type-2 Diabetes
It looks like men with fat bellies may not be all to blame for their expanding waistline. Researchers found that men with higher levels of chemicals found in colognes, plastic bottles, shampoos, deodorants and the plastics in the microwavecontainer may all be respsonsible. larger waist circumference and increased symptoms of type-2 diabetes. Men from the National Health and Nutrition Examination Survey were measured for waist size, insulin resistance and other tests of liver and kidneys. Results showed a significant increase in waist size with higher levels of phthalates. This was also true for a test determining insulin resistance which is what defines type-2 diabetes.
How Phthalates Actually Cause Diabetes Type-2
While we've described study after study linking phthalates with increased obesity and diabetes, the next question is why? How do these microscopic chemicals cause such chaos inside our bodies after hitching a ride in cosmetics, colognes, plastic covered food - plastic water bottles and plug-in air fresheners?
This 2017 study out of Anhui Medical University in China wanted to find out just this answer so researchers began by taking a group of adult male rats and dividing them into four groups. A normal group fed with regular diets and three groups exposed to the phthalate known as DEHP. The rats given DEHP received different doses of 0.05, 5 and 500mg/kg body weight. They also used liver cells in a test-tube setting and divided these into 6 groups, all receiving a different dose of DEHP. When the results were in - the DEHP-exposed rats exhibited many more problems than those receiving regular food. They experienced significantly increased liver damage, glucose tolerance, and insulin tolerance along with reduced expression of insulin receptor and GLUT4 proteins in the liver tissues. As a review here folks, you may remember that the insulin receptor is what lies on the outside of our cells to "catch" the insulin floating in your blood. Once the insulin is locked in, glucose can then be transported into the cell through the glucose "door" transporter called GLUT4. Results of the experiments with the liver and kidney cells showed that DEHP activated something called a peroxisome proliferator. All you need to know here is that this then resulted in another dominoe falling which started the production of compounds causing oxidative stress and also reduced the expression of the insulin receptor and GLUT4 proteins in liver cells. In other words, this is the first study we've seen that shows specifically how our everyday DEHP can cause a major malfunction of our insulin and glucose doors on the cell.
Cancer Treatments
Increase Diabetes and other Illnesses
The chemotherapy drug cyclophosphamide is known to cause diabetes in test animals. In fact, it is sometimes used to induce diabetes in animal studies. In this study, researchers wanted to find out if people treated with chemotherapy and/or radiation experienced higher rates of other illnesses after 5 years. A total of 14,290 patients from the Childhood Cancer Survivor Study participated in the project. The median age of the group was 6 years. Results showed that children exposed to "high risk" therapies (cyclophsphamide of 20/g/m(2) had nearly twice the rates of diabetes and twice the rates of obesity. Growth hormone deficiency was 5 times higher and thyroid cancer 9 times higher, Women had a six-fold increase in problems with their ovaries and men had higher rates of testosterone replacement.
Journal Clinical Oncology
vol. 34(27): 3240-32407, Sep 2016
University of Pennsylvania
Fred Hutchinson Cancer Research Ctr
St. Jude Children's Research Hosp
Common Food Pesticide DDE
Increases Diabetes
DDT is a pesticide that was banned in the U.S. in 1972, but is still used in agriculture settings in South America and in Africa for mosquito control. During the winter in the United States, upwards of 30% of produce is imported from South America and other countries is frequently found as a contaiminant in different food crops in grocery stores (i.e. lettuce). Along with DDT being used in foreign countries who send food crops back to the U.S., DDT is also a comtaminant in the U.S. pesticide dicofol (kelthane). So while DDT itself is banned in the U.S., it still can be applied to U.S. crops through the pesticide dicofol (especially cotton and citrus). Once DDT is applied, it forms the metabolite DDE. In this study, 619 sport fish consumers agreed to donate a blood sample in 1994-1995 and 209 participants donated again in 2001-2003. Health information was collected from each group. In total, 293 people from the original blood collection in 1994-95 provided a second sample for analysis in 2001-2005. Blood was tested for the pesticide DDE and PCB's. Participants who were without diagnosed diabetes in 1994-95 were followed for incident diabetes for an average of 8.4 years. Participants were then put into 3 groups of low, medium and high blood levels of DDE. Results showed a consistent dose-related association of DDE with incident diabetes. CHEM-TOX NOTE: We did a study in 1990's at the Florida Department of Agriculture in Tallahassee, Florida showing 19% of commercially grown lettuce tested in supermarkets contained the pesticide DDE. DDE is not found in significant amounts in organically grown produce.
Environmental Health Perspectives
Vol. 117(7): 1076-1082, July 2009
Mary Turyk, et al.
Division of Epidemiology & Biostatistics
School of Public Health
University of Illinois
Chicago, Illinois
The Chemical PCB in Older Homes
Linked to Diabetes
PCB is the abbreviation for the chemical polychlorinated biphenyls. It was well known for its use as a coolant in electrical transformers commonly seen on neighborhood telephone polls prior to 1980. What is not commonly known is that It was also used as a thickening agent in some paints, floor varnishes and caulking used in home construction. Some homes and schools built before 1980 have been found to have high levels of PCB's - some of which had to be demolished because of PCB levels. A severe outbreak of PCB poisoning affected thousands of Taiwanese people in the late 1970's. In a 24 year follow-up, researchers studied 1,054 of these victims for rates of diabetes. After adjusting for factors such as cigarette smoking, alcohol intake and BMI, it was found that women who had been exposed to the higher levels of PCB's had diabetes rates 5.5 times higher than people not exposed to PCB's.
Diabetes Care
Vol. 31(8):1574-1579, August 2008
National Health Research Institutes,
Miaoli, Taiwan
Corresponding Author:
Dr. Yueliang Leon Guo
DIOXIN - PCB's and Pesticide DDT
Strongly Linked to Diabetes
BACKGROUND: When testing the blood of people in most countries today - nearly everyone has measureable levels of the chemicals DIOXIN, PCB's and the pesticide DDT. Although PCB's and DDT have been banned in the U.S., higher blood levels of these chemicals can sometimes be found in people living in older homes built prior to 1990. DDT exposure can occur to people consuming foods imported from countries still using DDT (i.e. South America) and also from the pesticide Kelthane (which contains up to 5% DDT). Exposure to DIOXIN occurs from vehicle exhaust, burning of plastics, rubber and colored paper in trash and as an unintentional by-product in the manufacture of some pesticides used in agriculture and on lawns. In this study, conducted at the Medical University of South Carolina, researchers measured levels of these 3 chemicals in more than 1,800 people enrolled in the 1999-2002 National Health & Nutrition Examination Survey. Relationships of chemical exposure was then investigated for people with diagnosed diabetes, undiagnosed diabetes (HbA1c more than or equal to 6.1%) and total diabetes (diagnosed plus undiagnosed). Results showed that people with higher levels all three chemicals had significantly increased rates of diagnosed diabetes. In conclusion, the researchers stated,
These findings add to the list of chemicals found to be associated with diabetes in the 1999–2002 National Health and Nutrition Examination Survey.
Environmental Research
Vol. 103(3): 413-418, March 2007
Dr. Charles J. Everett
Medical University of South Carolina
Pesticide in Indoor Air of Older Homes
Linked to Diabetes
In a moment, you'll read how the pesticide chlordane is being linked to causing diabetes, however, before reading this, it is important to first understand that the majority of homes built before 1980 contain air levels of this banned pesticide. The problem even worse in homes built before 1979 when chlordane was used in routine indoor pest control. Unlike most pesticides today, chlordane does not break-down easily and continues to evaporate into the indoor air of older homes. The chemical heptachlor is commonly found as part of chlordane.
In a moment, you'll read how the pesticide chlordane is being linked to causing diabetes, however, before reading this, it is important to first understand that the majority of homes built before 1980 contain air levels of this banned pesticide. The problem even worse in homes built before 1979 when chlordane was used in routine indoor pest control. Unlike most pesticides today, chlordane does not break-down easily and continues to evaporate into the indoor air of older homes. The chemical heptachlor is commonly found as part of chlordane.
The associations of 8 pesticides and pesticide metabolites with total diabetes (diagnosed and undiagnosed) and pre-diabetes (glycohemoglobin 5.7–6.4%) were evaluated using the National Health and Nutrition Examination Survey (NHANES), 1999–2004. Six of the pesticides were found to be associated with total diabetes. These pesticides and pesticide metabolites were beta-hexachlorocyclohexane, p,p′-DDE, p,p′-DDT, oxychlordane, trans-nonachlor, and heptachlor epoxide. When the number of compounds elevated was tested, 4 or more, of the 6, elevated had an odds ratio of 4.99 (95% CI 1.97–12.61) compared to none elevated. When the 6 compounds were tested together in a single combined adjusted logistic regression only oxychlordane, a metabolite of chlordane, and heptachlor epoxide, a metabolite of heptachlor, were significantly associated with total diabetes. In the combined adjusted logistic regression, oxychlordane ≥ 14.5 ng/g lipid adjusted had an odds ratios of 1.90 (95% CI 1.09–3.32) compared to oxychlordane 14.5 ng/g lipid adjusted, and heptachlor epoxide ≥ 14.6 ng/g lipid adjusted had an odds ratio of 1.70 (95% CI 1.16–2.49) compared to heptachlor epoxide 14.6 ng/g lipid adjusted. Heptachlor epoxide and p,p′-DDT were significantly associated with pre-diabetes in separate adjusted logistic regressions. When these 2 compounds were tested together only heptachlor epoxide remained significantly associated with pre-diabetes. The evidence supporting the relationship between pesticides and pesticide metabolites, with diabetes, was strongest for heptachlor epoxide and oxychlordane, intermediate for p,p′-DDT, and least for beta-hexachlorocyclohexane, p,p′-DDE, and trans-nonachlor. Mirex and dieldrin were not associated with total diabetes or pre-diabetes.
Head Lice and Pet Pesticide Inceases Diabetes
The people of Saudi Arabia have one of the highest rates of diabetes in the world with over 30% of the adult population afflicted in 2010. With diabetes doubling every 12-15 years, along with the fact that their diabetes rates are already twice as high as the U.S., they are on an accelerated time-table for trying to figure this thing out. Unlike other pesticides that are typically applied away from the average person, pesticides used for lice are applied directly to a person's head and also applied to pets in shampoos and other forms as a flea and tick treatment. The extended time in treating a person or pet can expose the person running the operation to elevated levels of the chemical.
In this study, conducted at the College of Applied Medical Sciences in Saudi Arabia, researchers collected blood samples from 280 adults. About half had type-2 diabetes and the other half were healthy people without diabetes. Results were quite dramatic - Looking first at the 144 people without diabetes, it was found their average blood levels of the chemical was 3.8, while the average levels for those with diabetes was 8.8. To put this another way, the 136 people with diabetes had twice the amount of the chemical floating in their blood as the people who did not have diabetes.
It should be mentioned that the chemical Lindane was in the past used on farms and in lice and pet, flea and tick treatments. However, because of its high toxicity, many countries have banned it entirely. While it is banned in the U.S. for use on pets, seeds and farming, it still can be used in the U.S. but only as a second alternative for head lice removal if the first methods fail.
Common Disinfectant & Weed Killer
Linked to Diabetes
Dichlorophenol (DCP for short) is a chemical used in common weed killers and disinfectants used in hospitals, schools and homes. Exposure can also occur from drinking or showering with city water where chlorine is used for disinfection. To determine if the chemical was linked to diabetes, researchers at Mercer University Medical School in Macon, Georgia measured DCP levels in 560 adults with diabetes and 2,503 adults without diabetes. People were then divided into four equal groups from low to high depending on their level of DCP. After adjusting for age, weight, smoking and other factors, they found that people in the highest DCP group had a 59% higher rate of diabetes than those in the lower DCP group. They also found what is called a dose-response effect in that diabetes rates increased in four groups as DCP levels increased. the higher DCP group had significantly higher rates of insulin resistance. In conclusion, the scientists stated,
This study demonstrated a potential association between exposure to p-DCB, measured as urinary concentrations of 2,5-DCP, and diabetes in US adults.
Immune System's Natural Killer Cells Critical
for Protecting You from Diabetes
Mice were were exposed to environmental factors known to cause diabetes (i.e. cyclophosimide). It was found that some mice quickly developed diabetes and others showed no signs of diabetes. When looking at specifics in their immune systems, it was found that the mice who did not develop diabetes had higher numbers of natural killer cells and their natural killer cells also produced higher levels of interleukin-4 (IL-4). Interleukin-4 is one of the ways in which white blood cells communicate to other white blood cells.
CHEM-TOX COMMENT: As lower numbers of natural killer cells were shown to increase diabetes, this raises the question as to whether any environmental factors are present that lower the number and/or quality of natural killer cells.
Autoimmunity Improves
via Natural Killer T Cells
Natural killer T cells are slightly different than the more common natural killer cells. Natural killer T cells are far less common than natural killer cells and comprise only about 0.1% of all blood T cells. They have the unique ability to produce large amounts of cytokines (the immune system's communication chemical) which has the ability to communicate with other immune cells and also suppress immune system response. In studies of patients and mice with a variety of autoimmune diseseases, the number and functions of natural killer T cells is reduced. In experiments with mice, it was found that a deficiency of natural killer T cells worsens autoimmune conditions (such as diabetes). Therefore, one would expect that someone who has a lower number of natural killer T cells would have less suppression of autoimmune reactions within the body and consequently, a higher rate of tissue damage from autoimmune reactions within the body.
Current Molecular Medicine
Vol. 9(1): 4-14
Dept. of Microbiology & Immunology
Vanderbilt Univ. School of Medicine
Nashville, TN USA
Rapid Progression of Type-1 Diabetes
Occurs
if
patients have low numbers of some types of natural killer cells
Although the immune system's lymphocyte T cells play a key role in beta-cell destruction in the pancreas, researchers were finding other immune system cells were malfunctioning and contributing in the all out assault on the pancreas. Normally, cells called regulatory T cells (Tregs) and invariant natural killer T cells (iNKT for short) have the job of maintaining what is called "periperhal tolerance." This simply means their job is to insure everyone on the immune system team plays by the rules and and tolerates normal body cells. So, basically, the Tregs and iNKTs make sure everyone is friendly. However, in patients with type-1 diabetes, it was found their Tregs and iNKT's were lower in number and performing abnormally. In fact, when researchers artificially increased the number of iNKT cells in animal studies, the animals showed a decrease in type-1 diabetes. When mice had high levels of iNKT cells, diabetes wasn't a problem. In fact, researchers were able to pinpoint what was wrong with these previously normal functioning cells. Apparently, crowd control goes south with the cells no longer can produce enough of two compounds known as interleukin-13 and interleukin-14 - We'll call them IL-13 and IL-14 for short. Excuse this next analogy, but IL-13 is like mace that allows iNKT cells to calm down any other cells in the area that are thinking about attacking teh beta-cells in the pancreas. Although the authors in this study state there is no therapy to revent type-1 diabetes, they do state that if we can determine the origin (cause) of iNKT cell alteration, it would represent a new path to intervene before type-1 diabetes and the information provided in this book is attempting to do just that.
DIABETES (American Diabetes Assoc).
Vol. 65(8): 2121-2123, August 2016
These Immune Cells Both Destroy
and Protect the Pancreas
This study reviewed the research on how the immune system damages the pancreas.
While we hear much about autoantibodies, here are two key points from this article.
1. T Regulatory Cells (called Tregs) prevent diabetes (animals deficient have accelerated diabetes onset).
2. Patients with diabetes have impaired function of natural killer cells.
Nature Reviews Immunology
Vol. 10: 501, July 20, 2010
Immune cell crosstalk in T1D
Macrophage Malfunction:
1st Autoimmune Step to Diabetes Type-1
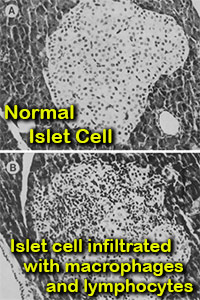
Macrophages are a type of white blood cell in the immune system.
In conclusion, the scientists stated, Along with cells called dendritic cells, macrophages are number 1 among cells that present signals (antigens) to other cells to mount an attack. Researchers in this study found an interesting observation among mice genetically prone toward diabetes type-1. When mice were exposed to a compound known to cause diabetes, the islets in their pancreas (islets hold insulin producing beta-cells) became flooded with macrophages and other immune system cells in a process known as insuliltis (see picture). They also found that by reducing macrophages (through exposure to silica), there was a dramatic decrease in function and numbers of T lymphocytes and natural killer cells - resulting in prevention of the pancreas beta-cell destruction. The authors quoted other studies showing that natural killer cells and helper and cytotoxic T lymphocytes are actively involved in the destruction of islet cells (paragraph 3, Pg.585).
On the basis of our earlier studies and this study, we conclude that the prevention of insulitis and diabetes in STDPBB rats (rats treated with silica) is due to a decrease in macrophage-dependent T lymphocytes, including helper/inducer and cytotoxic/suppressor, and NK cell cytotoxicity.
DIABETES
Vol. 39(5): 590-596, May 1990
Julian McFarlane Diabetes Research Ctr
University of Calgary
Alberta, Canada
Journal of Experimental Medicine
Vol. 189(2): 347, January 1999
Julian McFarlane Diabetes Research Ctr
University of Calgary
Alberta, Canada
How Natural Killer Cells & Thymus Gland
Prevent Diabetes & other AutoImmune Disorders
As described in the research above, islet cells in the pancreas are flooded with macrophages prior to development of diabetes and subsequent destruction of beta-cells. It has also been found that patients with diabetes and those with other autoimmune disorders are highly predisposed to the development of macrophage activation syndrome (MAS).
Below are the main points about this syndrome:
1. Macrophage activation syndrome is caused by hyperactivation of the macrophage immune response as a consequence of impaired natural killer cell function. In a population of patients with autoimmune disorders, type-1 diabetic patients are extremely predisposed to this syndrome. Pg. 472, par1)
2. Environmental factors are necessary to trigger the development of autoimmune disorders. Under normal conditions, the thymus prevents the complete development of autoimmune lymphocytes due to the mechanism of central tolerance. Nonetheless, small pools of autoreactive cells escape from the selection to peripheral circulation. As a back-up, there are also peripheral mechanisms (peripheral self-tolerance) aimed at destroying autoreactive lymphocytes. If central or peripheral tolerance mechanisms fail, immune reaction to self antigens can initiate autoimmunity [see study].
3. Natural killer cells have the ability to destroy lymphocyte cells attacking the pancreas. They do this by attaching onto the autoimmune T cell - and then releasing granules containing perforin and granzymes B into the T cell. This results in very fast destruction of the autoimmune T cell.
4. To quote the authors directly (pg471, par1), "Impaired action of perforin, disturbed degranulation process or defects in Fas/FasL-dependent apoptosis pathway may lead to the loss of natural killer cells function and to development of autoimmune disease.
Central European J Immunology
View Online -
Download PDF
Vol. 40(4): 470-476, Jan 2015
Medical University of Warsaw
Poland
Excellent Review of Natural Killer Cells
in AutoImmune Disorders
In another report, scientists conducted an extensive review of research investigating the role played by natural killer cells in protecting us from diabetes and other autoimmune disorders. Below are direct quotes from their report:
1. Cytokine activated human NK (natural killer) cells can directly kill both activated macrophages and T Cells.
2. Impaired NK cell function is frequently seen in patients with autoimmune disorders.
3. Over the last 30 years, many studies have reported decreased NK cell numbers or impairment of NK cell cytotoxicity in the peripheral blood of patients with autoimmune diseases such as multiple sclerosis (MS), rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), Sjögren's syndrome, and type I diabetes mellitus (T1DM)
4. ...more recent studies have also clearly identified an association between bona fide NK cell deficits in the peripheral blood with many autoimmune disorders [55] including autoimmune thyroid disease [56, 57] and psoriasis [58] as well as a number of pediatric rheumatologic diseases including juvenile dermatomyositis [59] and systemic-onset juvenile idiopathic arthritis (JIA) [60].
5. ...these reports raise the possibility that autoimmunity may be associated with NK cell numeric or functional deficiencies.
6. ...several studies have demonstrated accumulation of NK cells in affected tissues of autoimmune patients. For example, infiltrating NK cells have been found to accrue in the pancreatic islet of T1DM patients [64], the hair follicle of patients with alopecia areata [65], and the muscle of children with juvenile dermatomyositis [66, 67]
7. Interestingly, CD56 bright NK cells, in particular, accumulate in the skin lesions of psoriatic patients [68] and the synovium of RA patients [69, 70]. These observations support the hypothesis that decreased NK cells in the peripheral blood of patients with autoimmune disorders may reflect the trafficking of NK cells to affected tissues.
8. Furthermore, studies in T1DM have demonstrated modestly decreased NK cell numbers in the peripheral blood of patients with recent-onset T1DM but not in patients with long-standing T1DM [72]. Interestingly, NK cells were identified around the islet cells of a subset of patients with recent-onset T1DM [64] but not in postmortem pancreatic samples from T1DM patients with long-standing disease [73]. Murine models of T1DM have also demonstrated localization of NK cells near islets as well as a temporal correlation in NK cell infiltrates during the development of diabetes, with a greater influx of NK cells during the prediabetic stage compared with late diabetes [74, 75, 76].
9. ...chronic NK cell lymphocytosis (increased numbers of immature NK cells) is associated with autoimmune syndromes, including vasculitis, arthritis, and peripheral neuropathy [82, 83, 84]. This disorder provides evidence that the dysregulation of NK cell homeostasis in the context of decreased NK cell cytotoxicity may contribute to the onset of autoimmunity.
10. Natural Killer (NK) cell activation is regulated through several disinct mechanisms to prevent inappropriate responses. First, they express inhibitory recptors that recognize widely expressed ligands. Second, the up-greulaton of host ligands for activating receptors is regulated to prevent inadvertent damage to normal health tissue. Finally, full NK cell responsiveness requires "licensing" through inhibitory receptors, which prevents the unrestrained activation of NK cells that do not express appropriate self-MHC class I-reactive inhibitory receptors. For people without a degree in immunology, this simply means that natural killer cells possess several ways to prevent them from attacking healthy tissue.
Arthritis Research & Therapy
Vol. 15: 216, July 2013
Drs. L Fogel, W Yokoyoma, A French
Division of Pediatric Rheumatology
Washington University
Natural Killer Cells Destroy Macrophages
Linked to Starting Type-1 Diabetes
While the thymus gland works as the body's initial filter for removing autoimmune cells, there appears to be a "back-up" system ready to go in case the first defense goes on the blilnk. In this study, researchers demonstrated that human macrophages have the ability to activate natural killer cell proliferation and "prime" natural killer cells to kill target cells. On the flip side, they also found that natural killer cells also have the ability to directly kill autoimmune related macrophages. In conclusion the researchers stated,
These data suggest a new function for NK (natural killer) cell cytoxicity in eliminating overstimulated macrophages. This is important as overstimulated macrophages can be one of the first steps in pushing someone toward type-1 diabetes.
BLOOD
Vol. 109(9): 3776-85, May 2007
Division of Cell & Molecular Biology
Imperial College London, UK
While the section above described how defects in natural killer cell function can cause autoimmune disorders such as diabetes, this next section will investigate studies showing damage to natural killer cells from chemicals in the environment.
Natural Killer Cells Damaged by
Mosquito Control Pesticide Naled
Links to Diabetes and Autoimmune Disorders
Natural killer (NK) cells are critical for preventing viruses from host infection as well as preventing cancer. Loss of function or numbers of these cells increases rates of high viral prevalence and more aggressive cancers. NK cells have also been found to play a large role in preventing autoimmune disorders by attacking T cells showing autoimmunity toward the pancreas. Therefore, any situation that damages natural killer cell number or function has the potential for accelerating the onset of autoimmune disorders such as diabetes. .
In this study, scientists investigated if the pesticide dichlorvos (a breakdown product of Naled/Dibrom) and the common agricultural pesticide lorsban (chlorpyrifos) were able to damage natural killer cells. Natural killer cells were treated with both dichlorvos and chlorpyrifos at levels from 0 to 100 parts per million for 1 to 72 hours. Results showed that both pesticides caused destruction of natural killer cells through a process known as apoptosis in a time and dose-dependent manner. Chlorpyrifos showed a faster response than dichlorvos at higher doses; whereas, dichlorvos showed a slower, but stronger apoptosis-inducing ability at lower doses.
TOXICOLOGY
Vol. 239(1-2):) 89-95, July 2007
Dept. of Hygiene & Public Health,
Nippon Medical School,
1-1-5 Sendagi, Tokyo, Japan
Pesticides Weaken Ability of Natural Killer Cells
to Destroy Cancer
Same Pesticides found in Indoor Air of Homes
built before 1989
Alhtough this study is done with cancer and not diabetes, it is important to include here because it shows how natural killer (NK) cells can be damaged by pesticides and NK cells also play a critical role in protecting us from autoimmune diseases including diabetes.
NK cells play a central role in your immune defense against tumor development and viral infections. Thus, any agent that interferes with the ability of NK cells to lyse (kill) their targets could increase the risk of tumor incidence and/or viral infections [author quote from Abstract]
In this study, scientists tested 11 different pesticides to see if they were able to weaken the ability of natural killer cells to destroy cancer cells in a laboratory setting. The compounds were tested in both purified NK cells as well as a cell preparation that contained lymphoctye T cells) and NK lymphocytes (referred to as T/NK cells). Lymphocytes were exposed to the compounds for periods of time ranging from 1 hour to 6 days.
Results showed that exposure of highly purified NK cells to 5 microM of different pesticides for 24 hours greatly weakened their ability to remove and destroy cancer cells. Below is a breakdown of specific pesticides and their reduction in cancer killing capacity of the NK cells.
| alpha-chlordane |
88% reduction in NK killing ability |
| gamma-chlordane |
92% reduction in NK killing ability, |
| DDT |
61% reduction in NK killing ability |
| Heptachlor |
64% reduction in NK killing ability |
| Oxychlordane |
69% reduction in NK killing ability |
| Pentachlorophenol (PCP) |
76% reduction in NK killing ability |
The loss of cancer killing ability with alpha-and gamma-chlordane remained essentially constant for 6 days, while that seen with DDT, oxychordane and PCP increased with longer exposures. PCP was the most effective of the compounds tested at decreasing NK function. Of the compounds that caused decreased cancer killing when tested in purified NK cells, PCP and oxychordane also decreased the cancer killing ability of T/NK cell preparation. In conclusion, the researachers stated,
The results provide evidence of relative toxic potential for the 11 compounds and their immunomodulatory effects on other mononuclear cells (such as T-cells, B-cells, and monocytes) as well as NK lymphocyte function.
Department of Chemistry
Tennessee State University
Nashville 37209, USA.
CHEM-TOX NOTE: Of signficant concern, the pesticides chlordane and heptachlor are still routinely found in indoor air of homes built before the compound was banned in 1989. Also, homes built before 1980 have been found to have significantly high levels of chlordane and heptachlor as the pesticide was frequently used inside homes in monthly pest control operations.
Flame Retardant Severely Weakens Immune Natural Killer Cells
Journal of Immunotoxicology
Vol. 6(4), Oct 5, 2009
Triphenyltin Pesticide Causes Severe Damage
to Natural Killer Cells
Triphenyltin is a fungicide used in paints on the bottom of boats and as a pesticide in agriculture. In this study, scientists exposed freshly isolated white blood cell lymphocytes to triphynyltin compounds at levels of 750nM for 1 hour in a test tube. This resulted in a 63% decrease in natural killer cell cytoxic function. This means natural killer cells destroyed 63% less cancer or virus infected cells. Scientists then wanted to see if time would restore their ability. To test this, after exposure to the 750nM triphenyltin, they put the natural killer cells into a clean environment free of triphenyltin. After 6 days - results showed they had weakened even further and had a 91% reduction in cytotoxic ability.
CHEM-TOX COMMENT: Although not related specifically to diabetes, this study is included because of the critical importance being found of natural killer cells and their ability to eliminate autoimmune cells. Also, this study shows that while an initial test may not show immune system effects from a chemical, it is important to continue testing through a significant time period as effects can show up days following exposure.
Environmental Research
Vol. 92(3): 213-2120, August 2003
Dept. of Chemistry
Tennessee State University, USA
Diabetes Higher in People Exposed to
Chlorine Based Chemicals
Fascinating study in which 90 healthy non-diabetic young adults were followed for 23 years to to see who got diabetes later in life. Blood samples of the 90 individuals were tested in the mid-1980's (before beginning the study) for what is called "persistent organic pollutants" (We'll call it POP for short.) POPs are chemicals that typically do not break down easily and remain toxic for many decades. There were 55 different POP chemicals tested including organochlorine pesticides - chemicals used as flame retardants and chemicals known as PCB's. PCB's were used as a thickening agent in construction materials such as caulking, varnishes and paints in homes built in the 60's and 70's. In fact, organochlorine pesticides and PCB's are typically found at much higher concentrations in homes built before 1989 than homes built after this date. This is because some of the most toxic POPs were banned in 1980 and 1989. Results of this study found that people who had higher levels of organochlorine pesticides and PCB's in early adulthood had significantly decreased insulin sensitivity after they reached 40 years of age. In conclusion, the researchers stated,
Our findings suggest that impairments of glucose metabolism occur after decades of exposure to PCBs and organochlorine pesticides at background levels, independent of BMI and after participants reached the 5th decade of life.
Environmental Research
Vol. 137: 485-494, Feb 2015
Department of Family and Preventive Medicine, University of California
Department of Preventive Medicine, Kyungpook National University, Korea
Hospital del Mar Institute of Medical Research (IMIM),
School of Medicine,
Universitat Autonoma de Barcelona, Barcelona, Catalonia, Spain
Department of Laboratory Medicine and Pathology, University of Minnesota, USADivision of Epidemiology and Community Health,
University of Minnesota, Minneapolis, MN, USA |
Astounding 38-fold Increase in Diabetes for the 10% of the Population with the Highest Levels of Six Chemicals
The majority of medical studies discussed in this book show increased diabetes rates of 30% - 50% and even several hundred percent after exposure to a single or several chemicals in a particular consumer product. In this study from the University of Minnesota and Kyungpook University in Korea, researchers decided to investigate the effects of chemicals in combination that are also known to have diabetes promoting effects individually. This type of study design represents more closely to what all of us experience daily.
Using blood samples from 2,016 adults from the 1999-2002 National Health and Examination Survey, researchers looked for the presence of six different chemicals. Scientists wanted to determine if people with higher levels of these chemicals had higher rates of diabetes. Chemicals tested included the food and termite pesticide chlordane, the electronic and construction chemical PCB's (used in caulking and paint of older homes), the food pesticide DDE (in non-organic foods imported from South America), and several types of Dioxin (found in vehicle exhaust, trash burning and some pesticides). The chemicals were selected because they are commonly found in 80% of the population.
Scientists measured the levels of these six chemicals in each person's blood and then added them together to give a total chemical exposure dose. Results for the total chemical dose in these 2,016 adults were then divided into five separate groups - starting with the lower exposure group (for people with the lowest levels of total exposure dose) and gradually increased for groups with higher total levels of the 6 chemicals. Results were divided along percentiles - 25th, 50th, 75th and 90th percentiles.
When comparing diabetes rates in each group, it was found that people in Group 2 (25th to 49th percentile) had an astounding 14 times higher rate of diabetes than those in the lowest Group 1. Continuiing this further, those in the highest chemical exposure Group 5 (those above the 90th percentile) had a 37.7 higher rate of diabetes than Group 1. The dramatically increased rates of diabetes for people with higher levels of these chemicals is unprecedented and points the finger straight to what is causing the massive increase in diabetes we are seeing today. In conclusion, the researchers stated,
Chronic exposure to low concentrations of POPs (persistent organic pollutants) in the general population may be more detrimental in developing adverse health effects than previously thought
Because of the importance and magnitude of these findings, it is important to discuss not just the names of chemicals increasing diabetes rates, but also, what consumer products and situations where you could be exposed to these chemical combinations. Although you won't find this information in the current study, we've done the homework for you below:
1. PESTICIDE CHLORDANE (Main Source: Older Homes & imported non-organic food)
Chlordane was routinely used as a termite treatment chemcal in foundations of homes built before 1989. It was banned because it was found to enter the interior air breathing space decades after application and was linked to many health problems and cancer. The problem is worse in homes built before 1980 in which it was used inside homes for the treatment of roaches, ants, etc.
2. PCB's (Main Source: Older Homes built before 1980)
Used in older power transformers seen on telephone polls as a cooling liquid, it was also used extensively in caulking, paint and varnishes of older homes built in the 60's and 70's. Small, but toxic levels continue to be emitted into the air of older homes which can be inhaled by occupants and gradually build up to higher levels over the years in the person's fat tissue.
3. DIOXIN (Main Source: Vehicle Exhaust - Waste Incineration - Trash Burning)
Formed as a by-product when making some pesticides, dioxin is also formed during vehicle engine combustion and then inhaled by people driving on highways or those living near roadways. High levels of dioxin are also formed from waste incinerators and when homeowners burn trash containing plastics, chlorinated white paper and colored ink magazine paper. Very high levels of the most toxic forms of dioxin are formed when burning rubber insulation covering metal wires.
4. DDE (Main Source: Pesticides in Food)
The chemical DDE is the main breakdown compound of the pesticide DDT. Although DDT was banned in the U.S. decades ago, the general population still gets exposed to it in several ways. It is formed as a by-product in the manufacture of the pesticide known as dicofol. Other main routes of exposure come from non-organic food imported into the U.S. from countries in South America. For example, when South American farms use DDT, it soon breaks down to DDE. Foods with DDE are then exported into the U.S., (especially during the winter) and the chemical is then ingested by the consumers in the U.S., Europe and other countries. DDE is a chlorinated fat soluble chemical which leads to higher and higher levels of this chemical in your body as long as you continue to eat non-organic food. Why DDT is banned in the U.S. but allowed to be sprayed on food in other countries and then imported back to the U.S. is a scratch your head type question, so you need to ask your congressman about that one...). One way to quickly reduce DDE levels in your body is to consume only organic foods which are grown without pesticides. Doing so now would then appear to significantly decrease your risk of diabetes, since people with lower levels of DDE have significantly lower levels of diabetes.
CHEM-TOX COMMENT: As most of these chemicals are more common in older homes, it generates an additional chemical burden for people living in poverty who typically reside in older dwellings. Also, families with less income are more inclined to burn household garbage rather than pay for municipal trash removal services, thereby further increasing exposure to dioxin compounds. Another observation from the study was that the older the person, the higher the levels of chemicals, which makes sense that more exposure over time would increase the body burden of these chemicals.
Diabetes Care
Vol. 29(7): 1638-1644, July 2006
Duk-Hee Lee, MD, PhD
In-Kyu Lee, MD, PhD
Michael Steffes, MD, PhD
School of Medicine
Kyungpook National University, Korea
University of Minnesota, USA
Diabetes on Track to Bankrupt the U.S. Economy if Not Reversed
As shown in the first journal summary from the CDC, diabetes has increased at least 7 fold from 1960 to 2014, going from 1% to 7%. If we count people with undiagnosed diabetes and those over age 20 it is over 12%. In a report published by the American Diabetes Association, the economic burden associated with diabetes (all ages) - prediabetes - and diabetes in pregnancy exceeded $322 billion in 2012, consisting of $244 billion in excess medical costs and $78 billion in reduced productivity. This is 48% higher than the $218 billion cost in 2007. The cost per person with diabetes averaged $10,970 per year for diagnosed diabetes, $5,800 for diabetes in pregnancy and $4,030 for undiagnosed diabetes and $510 for prediabetes.
CHEM-TOX COMMENT: If the trend continues, diabetes will double again in another 10-15 years by 2025 or 2030, resulting in 20% or more of the population with diabetes (and these may be underestimates). It will then double again 10-15 years later resulting with 40% of the population having diabetes by 2040 or 2045. Certainly, having 40-50% of the population with diabetes is financially unsustainable in any society as diabetes is a very costly illness at about $1000 per month. If diabetes doubles again 10-15 years then 80% or more of the population will have diabetes by 2055.
Diabetes Care
American Diabetes Association
Vol. 37(12): 3172-3179, Dec 2014
Pre-Diabetes Predicts Explosion
of Diabetes in 10 years
While CDC estimates for the year 2014 show about 12% of the U.S. population had diagnosed or undiagnosed diabetes, it has also been found that about 30% of the adult population (86 million) had pre-diabetes according to a report on the CDC's website - see report. Prediabetes is defined as a fasting blood glucose level of between 100 and 125. This is of great concern as other research from the European Diabetes Association show the majority of people with pre-diabetes develop diabetes within 10 years. Therefore, if 12% of the adult U.S. population in 2016 has diagnosed or undiagnosed diabetes, and another 30% of those remaining have prediabetes, we could conservatively say in 7-10 years - that another 20% of the U.S. population will have diabetes on top of the current 12%, resulting in more than 30% of the U.S. population having diabetes in 2025-28. This numbers are much higher than current predictions. If the rates continue, then, by at least 2045 or 50, more than half the U.S. population will have diabetes. With reports showing the cost for a person with diabetes is about $12,000 per year - the financial costs for treating half the population with diabetes would be financially unsustainable resulting in a complete collapse of the current medical insurance finance system.
30% Increase in Diabetes Close to Highways
People living closer than 330 feet (100m) from a major highway had more than a 30% higher risk of developing diabetes than people living more than 660 feet (200m). Researchers from a number of universities in Germany followed 3,607 individuals without diabetes in 2000-2003 in Germany for an average of 5.1 years and then compared rates of diabetes for the two groups.
Environmental Health
Vol. 14: 53, June 2015
Leibniz Research Institute for Env Med
Medical School, Einrich Heine University
Car Exhaust Chemicals
Increase Type 2 Diabetes in Older Women
Another study linking chemicals in car exhaust with diabetes was found among women age 54 and older. In this German study, 1,775 elderly women who completed the study were measured for diabetes over a 16 period from 1990 to 2006. Researchers found that women with diabetes had increased exposure to air pollutants (primarily from vehicle traffic), For example, of the 1,588 women who did not have diabetes after 16 years, their exposure to the car exhaust compound nitrous oxide was 11.7 tons per year per square kilometer while those who did develop diabetes were exposed to nearly 13 tons per year. A similar patter was also seen for the tons per year of PM from vehicle traffic as well. In conclusion, the researchers stated,
To the best of our knowledge, this is the first prospective, population-based study that showed a statistically significant association between traffic-related air pollution and incident type 2 diabetes.
Environmental Health Perspectives
Vol. 118(9): 1273-1279, Sep 2010
German Diabetes Center
Institute for Clinical Diabetology
Center for Diabetes Research
Heinrich Heine University
Dusseldorf, Germany
Moving from Low Traffic to High Traffic Area
Reduces Beta-Cell Insulin Output
While other studies have shown that people living close to highways had higher rates of diabetes, in this study, scientists wanted to see if diabetes markers would change if people moved from a rural country setting to a higher traffic setting in a city environment. To test this, 25 healthy adults living in rural Michigan were transported to a city location for 5 consecutive days of daily 4-5 hour-long ambient air pollution exposures. All participants were given tests for insulin resistance 7 days prior to the start of the test, then again on the last exposure day and again 7 days after completion. The levels of the automobile pollutant known as fine particulate matter 2.5 was also measured at the homes of the participants and at the city testing sites. Results showed that moving to the higher traffic areas in the city did in fact significantly reduce insulin resistance and reduced beta cell function. For each 10 µg cubic meter increase in the particulate matter 2.5 resulted with an increased score of 0.7 on what is known as the homeostatsis model assessment of insulin resistance. In conclusion, the researchers stated:
Our findings suggest that ambient particulate matter 2.5, even at low levels, may reduce metabolic insulin sensitivity supporting the plausibility that air pollution could potentiate the development of DM (diabetes mellitus).
General Air Pollution Worsens Metabolism in Children
Not only does car exhaust worsen symptoms of diabetes and glucose metabolism, but apparently, our general background levels of air pollution (coming primarily for coal and oil power plants) are contributing as well. In this study, scientists wanted to see how children's health was affected by general air pollution and traffic air pollution. had on 429 obese and overweight children in Los Angeles, California..but In conclusion the researchers stated,
"Elevated air pollution was associated with a metabolic profile that is characteristic of increased risk for type 2 diabetes. These results indicate that increased prior year exposure to air pollution may adversely affect type 2 diabetes-related pathophysiology in overweight and obese minority children."
Exposure to any Pesticide
Increases Diabetes by 61%
In a review of studies done on more than 80,000 individuals, it was found that exposure to any pesticide increases the risk of diabetes by nearly 61%. The lead author of the study, Dr. Fotinia Kavvoura, MD, PhD, presented this information at the 2015 annual meeting of the European Association for the Study of Diabetes (EASD). Dr. Kavvoura stated the study was done to understand what has been causing the exponential increase in type 2 diabetes in recent years. Along with these conclusions, it was also reported that women exposed to organic pollutants in early pregnancy had a fourfold increased risk of gestational diabetes compared with those who were not exposed to the chemicals. Organic pollutants include chemicals such as PCBs and are found in the air of older homes because of extensive use in caulking, floor varnishes and some paints.
Diabetes/Pre-Diabetes 11x Higher
in Mosquito Control Applicators
Rates of diabetes and pre-diabetes were 11 times higher in 116 men employed as pesticide sprayers in public mosquito vector control programs in Bolivia. The rate of diabetes and prediabetes was 61% among men employed to spray pesticides and only 8% among 92 non-exposed controls of the same age. A dose-response relationship was also found showing that pesticide applicators reporting the highest number of hours spraying had diabetes and prediabetes rates 14x greater.
Journal of Agromedicine
Vol. 19(4): 417-26, 201
4
Section for Env, Occup. & Health
Department of Public Health
Aarhus University,
Aarhus, Denmark
Farm Pesticide Applicators
Have Higher Rates of Diabetes
33,457 white males were enrolled in the Agricultural Health Study. Rates of diabetes were determined when beginning the study and again 5 years later in a follow-up interview. Workers reported types of pesticides used and how often. Seven pesticides were associated with increased risk of diabetes including aldrin, chlordane, heptachlor, dichlorvos (Naled), trichlorfon, alachlor and cyanazine). The odds of getting diabetes increased with using the pesticide only once and became higher with cumulative days of use. For example, applicators with more than 100 lifetime day use of the pesticide aldrin had a 51% increase odds of diabetes - those using chlordane had a 63% increased risk - and those using heptachlor had a 94% increased risk of diabetes. Increased risk of diabetes was also seen among organophosphate pesticides such as the agriculture and mosquito control pesticide dichlorvos (a break-down product of Naled). We found that applicators exposed to dichlorvos had an increased odds of diabetes and that the odds increased with increasing cumulative days of use, although the test for trend was only moderately significant. Furthermore, the pesticide most strongly associated with diabetes among applicators was the organophosphate insecticide trichlorfon, which is converted to dichlorvos in mammals (see study).
Major Breakthrough
in Understanding Autoimmunity?
Chemicals Attach to Proteins: 1st Step in Autoimmunity Process
PREFACE: It is well documented that a weakening or defective thymus gland loses its ability to filter (remove) autoimmune cells from the blood, thereby resulting in increased autoimmune cells remaining in the body resulting in increased damage to healthy tissue, and increased risk of diabetes. Evidence also shows that natural killer cells can attack and destroy autoimmune cells, thereby helping to reduce an autoimmune problem. However, natural killer cells can lose their ability to function properly when exposed to different petroleum chemicals, including some pesticides. The question still remains on what happens first in the body that causes immune system cells to become "ignorant" and begin attacking healthy tissue. In this 2015 study, scientists at the Immunosciences Lab in Los Angeles have for the first time provided evidence on what may be happening within the body to start of the autoimmune process. This was all done by documenting immune system responses to 11 common chemicals and comparing this with immune responses to a common mold called aflatoxin. Aflatoxin can produce toxic compounds and is found in small amounts in foods such as grains and peanuts. Once aflatoxin enters the body, it has been shown to bind with proteins in the blood (such as albumin) which then attach to healthy tissue. Immune system antibodies are then formed to attack this newly formed aflatoxin/protein combination, thereby causing an autoimmune response. Many chemicals used in consumer products and modern society are also being found to attach to proteins in the body prompting scientists to wonder if the autoimmune process that occurs from aflatoxin could also ocur from any of 11 common chemicals. To explore this theory, scientists took blood samples from 400 healthy donors and exposed each sample to aflatoxin and then to 11 different chemicals. This included the chemical known as BPA (used in making plastic bottles and food can liners), the pesticide permethrin (used in indoor pest control - mosquito control and agriculture), a common flame retardant chemical used in computer circuit boards and also a benzene type chemical commonly found in car exhaust, gasoline and some food coloring (i.e. yellow dyes). Scientists then measured specific antibodies that were formed after exposure to the chemical/protein combination and compared it to the level of antibodies formed after exposure to aflatoxin. The logic here being that if the chemicals caused the formation of similar levels of antibodies as did aflatoxin, then we could expect similar harmful autoimmune response from the chemicals. After exposure to aflatoxin, blood samples showed an average 7% increase for both IgG and IgM antibodies. Interestingly, some of the 11 chemicals caused similar or greater immune responses. For example, the water bottle chemical BPA resulted in an average increase of 13% antibodies for IgG and IgM. The benzene ring chemical (as in gasoline and vehicle exhaust) resulted in an average 11% increase in antibodies. The flame retardant chemical used in computers resulted in an average increase of 15% for IgG and IgM antibodies. The pyrethroid pesticide permethrin had one of the largest increases averaging about 19% for both IgG and IgM antibodies. As can be seen here, the levels of antibodies against the chemicals increased which supports the idea that common chemicals may be a significant contribution to in the increasing rates of autoimmunity (and potentially diabetes). In conlusion the researchers stated,
Currently, the pathological significance of these antibodies in human blood is still unclear, and this protein adduct formation could be one of the mechanisms by which environmental chemicals induce autoimmune reactivity in a significant percentage of the population.
Journal of Applied Toxicology
Vol. 35(4): 383-397,
April 2015
Immunosciences Lab, Inc.
Los Angeles, CA, USA
Dept. of Clinical Sciences
Bastyr University California
Dept. of Mathematics
Boise State University, USA
Chemicals in Dish Soaps - Laundry Detergents - Fragrances & Plastics
Alter Estrogen in Body Critical for Normal Insulin Levels
Many chemicals used in society are now being labeled as Endocrine Disrupting Chemicals (EDC). These chemicals mimic important homones in the body (such as the female sex hormone estrogen) and have been found to reduce the effects of estrogen in the body. Scientists at the School of Publich Health at Tongji Medical College in China wanted to investigate if the class of of chemicals called phenolic estrogen pollutants (used in many consumer products) could affect pancreas islets and beta-cell function in rats. Chemicals tested were octylphenol, nonylphenol and bisphenol A (BPA). Nonylphenol is used used in laundry and dishwashing detergents, rubber, vinyl, personal care products and paints. Octyphenol is used in the making of fragrances, flame retardants, carbonless pape and as an additive in gasoline. BPA is used in common water bottles and readily leaches into the water. Results of this study showed all three chemicals weakened mitochondrial function in beta-cells and caused "remarkable" swelling of mitochondria and disruption of genes responsible for proper beta-cell function. Researchers stated that physiological levels of estrogen are involved in maintaining normal insulin sensitivity, but an excess of estrogen, such as from exposure to chemicals with estrogenic activity, would increase the risk of developing insulin resistance and diabetes. The chemical BPA (used in plastic bottles and as a liner in canned food) had the lowest estrogenic activity of the four phenolic estrogens, but was able to significantly increase insulin release at a dose as low as 0.1 μg/l with 16.7 mM glucose stimulation, which means that BPA would affect insulin secretion within the environmental concentration range. These data suggest that BPA has more effect on disrupting insulin secretion and content in isolated beta-cells than those with higher estrogenic activity, which also indicates that the ability of the phenolic estrogens to disrupt insulin secretion is not positively correlated with their estrogenic activity.
Journal of Endocrinology
Vol. 215: 303-311, November 1, 2012
Key Laboratory of Environmental Health
School of Public Health
Tongji Medical College
Plastic Liner in Canned Food & Soda
Increases Diabetes & Heart Disease
The next time you pop open a can of vegetables - take a peek at the metal inside. While you will see the metal, you won't see something that is worrying scientists. Over top of this metal interior is a plastic coating made from the chemical bisphenol-A (also called BPA). The problem is that BPA leaches out of the liner and into the food while the can sits on the shelf. When the canned food is eaten, you then swallow small amounts of this chemical with every bite. The problem is BPA is a professional copy-cat of other important hormones in your body and has the ability to change levels of natural hormones controlling critical processes in the body. To determine if so-called normal levels of BPA found in people can affect the risk of diabetes, researchers from the United Kingdom looked at urine concentrations of BPA in 1,455 adults aged 18 through 74. Once BPA levels were measured, they divided results into 4 equal groups from lowest to highest BPA levels. After taking into account the person's age, race, weight and many other variables, they found that people in the highest BPA group had more than twice as many people with diabetes as those in the lowest BPA group. A significant increase in heart attacks was also found in the higher BPA group as well. In conclusion the researchers stated:
Using data representative of the adult US population, we found that higher urinary concentrations of BPA were associated with an increased prevalence of cardiovascular disease, diabetes, and liver-enzyme abnormalities.
BPA Also Changes Insulin Secretion
While the study above shows increased risk of diabetes with higher bisphenol-A (BPA) levels in the body, it is also important to find out why this might be happening. To briefly review how you get exposed to BPA, primary exposure comes from plastic liners in canned foods, aluminum soda and beer cans, food packaging, reusable water bottles (often marked with a #7 or "PC"), baby bottles, fast food, dental sealants applied to teeth and even cash register receipts. It is also used in computer circuit boards which, upon becoming warm, can emit the chemical into the air.
In this study, conducted at McMaster University in Canada, researchers tested six different chemicals for their ability to alter insulin secretion. Results showed only BPA directly affected insulin secretion. In conclusion, the researchers stated:
These data suggest that long-term BPA exposure may be detrimental to beta cell function and ultimately be an important contributor to the
eetiology of Type 2 Diabetes.
Another Way BPA Can Cause Diabetes - Autoimmunity
While type-1 diabetes was originally believed to be the type associated with autoimmunity, newer studies show type 2 diabetes is also affected by autoimmunity (although affecting different cells in the body). As you should know by now - an autoimmune reaction is when your immune system mistakenly attacks healthy tissue in the body. As the chemical BPA has been linked with increasing diabetes and affecting insulin output, researchers at Bastyr University in San Diego, investigated the current state of research on BPA and autoimmunity. They stated that many known autoimmune triggering mechanisms have been correlated with BPA including disruption of liver enzymes, macrophage activation (a type of white blood cell) and others.
Canned Food - Plastic Bottles
BPA Damages Critical Organ Protecting Us
from Diabetes: Potential for Increased Diabetes
in Children & Autoimmunity
Type-1 diabetes is growing faster in children under age 5 than any other age group. This means more children will suffer from the debilitating effects of diabetes and for a longer duration of their lives. Finding out the reasons for this increase is certainly of great importance for us and our children. A number of studies have been done (including ones discussed previously) linking the common chemical BPA with the increasing rates of diabetes. Along with the primary exposure sources of BPA (canned food & drinks), the chemical is also used in plastic baby bottles and leaches out faster when heated (as is often done with baby bottles). This gives a greater likelihood of increased BPA exposure in most children in society today. It's important to understand that your thymus gland is your body's first defense for removing autoimmune cells than can cause diabetes (even type-2 diabetes has now been linked with autoimmunity). Also, a number of modern chemicals have now been found to weaken the ability of your thymus to remove autoimmune cells. To determine if BPA could also affect development of the thymus, researchers divided 30 chick embryos into three groups of ten eggs each. On fertilization day 9, one group was injected with low levels of BPA (250 micrograms per egg), another group of eggs with a saline solution and the third group with corn oil. Thymuses were collected on day 22 and weighed. They were then looked at using a light microscope for any signs of damage. Results showed that the thickness of the thymus cortex and medulla was significantly reduced (showing damage to the thymus). Further investigations with an electron microscope showed that the lymphatic follicles and eptihelial cells of the embryos were damaged in the BPA group, but not the others. In conclusion, the researchers stated:
Our study confirms a direct toxicity of BPA at a very low-dose level on the development of the central immune organs of SPF chick embryos.
BPA Mimics Hormone Estrogen
Disrupts Pancreas Beta-Cell Function
The common chemical BPA is believed to mimic the hormone estrogen. In other words, BPA fools the body into thinking it is the hormone estrogen. This chemical masquerade can have very serious consequences in any person with the potential for causing many ill effects.
In this this current study, scientists wanted to compare how both BPA and estrogen could affect insulin output. They began by exposing adult mice to a single low dose of the estrogen compound estradiol. This resulted in a rapid rise in insulin and immediate decrease in glucose. Next, mice were exposed to the same level of BPA which resulted in the mice same change in insulin & glucose asd seen with estradiol. Scientists then continued the experiment by giving daily low dose exposures to different groups of mice with either BPA or estradiol. After 4 days of treament, both the BPA and estrogen treated mice developed chronic high glucose as well as abnormal results on both glucose and insulin tolerance tests. In conclusion the scientists stated,
These experiments unveil the link between environmental estrogens and insulin resistance. Therefore, either abnormal levels of endogenous estrogens or environmental estrogen exposure enhances the risk of developing type 2 diabetes mellitus, hypertension, and dyslipidemia.
JAMA (Journal of American Med. Assoc.)
Vol. 300(1): 1303-1310, Sep 2008
Epidemiology & Public Health
Peninsula Medical School
United Kingdon
International Journal of Toxicology
Vol. 30(4): 410-418, August 2011
Dept. of Obstetrics & Gynecology
McMaster University
Ontario, Canada
Autoimmune Diseases
Vol. 2014 (2014), April 2014
Division of Sciences
Bastyr University
San Diego, CA, USA
Toxicology Industrial Health
Vol 30(3): 199-205, July 2012
Dept. of Veterinary Pathology
China Agricultural University
Beijing, China
Environmental Health Perspectives
Vol 114(1): 106-112, Sep 2005
University Miguel Hernandez de Elche
Alicante, Spain
Fat Cells Exposed to BPA Grow Faster!
 While the chemical BPA has been linked with increasing obesity in a number of studies, this is the first study we've seen that was able to measure how much fat cells actually grew after exposure to BPA. Since humans could not be involved in a study of this design, scientists took cells from mice that normally grow into fat cells - scientists call them adipocytes. Since adipocytes and fat cells are the same thing we'll go with "fat cells" to save energy in pronunciation. The experiment worked like this: Scientists in Italy at the Federico University of Naples first treated a group of mouse pre-fat cells (called fibroblasts) with low levels of BPA for 2 weeks. The level of BPA is said to be what most of us are exposed to during our daily routine. On the beginning of the 15th day of the experiment, the pre-fat cells were placed into six separate plates for growing and observaton. At the end of 24 hours on day 16, the number of cells were counted and photographed. This was done again on day 17 and day 18.
While the chemical BPA has been linked with increasing obesity in a number of studies, this is the first study we've seen that was able to measure how much fat cells actually grew after exposure to BPA. Since humans could not be involved in a study of this design, scientists took cells from mice that normally grow into fat cells - scientists call them adipocytes. Since adipocytes and fat cells are the same thing we'll go with "fat cells" to save energy in pronunciation. The experiment worked like this: Scientists in Italy at the Federico University of Naples first treated a group of mouse pre-fat cells (called fibroblasts) with low levels of BPA for 2 weeks. The level of BPA is said to be what most of us are exposed to during our daily routine. On the beginning of the 15th day of the experiment, the pre-fat cells were placed into six separate plates for growing and observaton. At the end of 24 hours on day 16, the number of cells were counted and photographed. This was done again on day 17 and day 18.
 Results showed a number of major differences between fat cells exposed to BPA and fat cells not exposed to BPA. First, fat cells exposed to BPA were only able to use half as much glucose as those not exposed to BPA, thereby giving evidence of insulin resistance.
Results showed a number of major differences between fat cells exposed to BPA and fat cells not exposed to BPA. First, fat cells exposed to BPA were only able to use half as much glucose as those not exposed to BPA, thereby giving evidence of insulin resistance.
Below are a number of quotes by the authors:
In the current study, we have observed that prolonged exposure to low doses of BPA affected adipocyte differentiation program, by increasing pre-adipocyte growth and by altering master regulatory genes of adipogenesis.....
Newsworthy, it has been recently postulated that metabolic diseases, including obesity and diabetes, may originate from developmental defects, even occurring in fetal life, that can be worsened by later environmental challenges [18,19,41–46]. Indeed, considering that fetal life is a critical window for the adipose tissue development, our data are in agreement with the hypothesis that the early chronic exposure to low BPA doses could be responsible for alteration in genes, involved in adipogenic commitment and adipocyte differentiation, with possible adult-onset of metabolic alterations. Thus, BPA may both enhance the expansion of adipocyte precursors and increase lipid content.
However, adipose tissue turnover also occurs in adult life [22]. Therefore, the disrupting effect of prolonged BPA exposure cannot be excluded even in adult adipose tissue.
...to reduce BPA environmental chronic exposure would be beneficial to protect vulnerable individuals, such as pregnant women, infants and children and to prevent metabolic dysfunctions and negative outcomes later in the offspring life.
Mounting evidence strongly suggests that BPA may affect adipose tissue development and function, supporting the “environmental obesogen hypothesis” [3,35]. In the current study, we have observed that prolonged exposure to low doses of BPA affected adipocyte differentiation program, by increasing pre-adipocyte growth and by altering master regulatory genes of adipogenesis.
This BPA dose was chosen also based on dose-response experiments (not shown) indicating that lower doses (0.1 nM) were ineffective while higher doses were cytotoxic. Moreover, Schönfelder et al. and Padmanabhan V et al. [36,37] have reported a median BPA concentration in fetal and maternal blood of 22 ng/ml, even higher than 0.23 ng/ml (1nM).
Cigarette Smoke Increases Insulin Resistance Worsens Diabetes
This study included 34 patients who quit smoking and were followed for 1 year and continued not to smoke during the 1 year. 7 subjects had type-1 diabetes and 27 had type 2 diabetes. Mean A1c was 7.7 while smoking and 7.0 after stopping smoking.
Second Hand Smoking Increases Diabetes in Children & Adults
Women with at least one parent who smoked cigaretees had an 18% higher rate of type 2 diabetes than women whose parents did not smoke. When looking at adults exposed to cigarette smoke from their spouse, the increased risk of diabetes was 36%. This study was done with 37,343 French women who never smoked but who reported that one of their parents did smoke.
Diabetes Care
Vol. 36(9): 2720-2725, Sept 2013
National Institute of Public
Health
Mexico City, Mexico
Harvard School of Public Health
Boston, Massachusetts
Smoking More = Higher Rates of Diabetes
Quitting Reduces Risk of Diabetes
Of those smoking more than 2 packs per day, men had a 45% higher rate of diabetes and women had a 74% higher rate. Quitting smoking reduced the rate of diabetes to that of non-smokiers after 5 years in women and after 10 years in men. Researchers went on to state that a dose-response relationship seems likely between smoking and the incidence of diabetes. Smokers who quit may derive substantial benefit from doing so.
NEW: Beta-Cell Loss Not as Bad as Believed
Insulitis is the "hallmark" of type-1 diabetes. This is where immune system cells enter the islet and are suspected of causing damage. While insulitis is a critical element in type-1 diabetes, it is typically present only in a modest proportion of islets at any given time, even at diagnosis. The relative importance of of insultis as a determining factor in diabetes symptoms at disease onset appears to have been overestimated; growing evidience also shows that beta cell loss at diagnosis is more modest than previously thought. Thus, the sole targeting of the immune system may not afford full therapeutic efficacy if dysfunction affects beta-cells that are not under immune attack and this is a key contributor to symptoms. Combination therapies that promote both immunoregulation and address beta cell dysfunction should be more effective in treating this chronic disease process. Two distinct patterns of insulitis were described in autopsy samples from UK patients with recent onset T1D according to the prevalence of CD20 B-cells (CD20Hi and CD20Lo) [22]; these findings were replicated in the nPOD and DiViD cohorts [23]; the CD20Hi profile appears associated with an early age of diagnosis (7 yr) while those diagnosed after age 13 have a CD20Lo insulitis. Thus, the presence of higher proportions of B-cells in the insulitis lesion may be a marker of early triggering of autoimmunity or of a more rapid rate of beta cell loss..
Pediatric Diabetes
ABSTRACT -
FULL TEXT
Vol 17: Suppl 22: 31-36, July 2016
Diabetes Research Foundation
Miami, FL
Don't Assume: 90% Loss of Beta-Cells Not Correct
Latest Research shows only 40-60% Loss for Type-1
Doctors typically tell newly diagnosed type-1 diabetes patients that the disease occurs after 90% loss of beta-cells. While this was the previous belief, the latest studies on investigating deceased children with recently diagnosed diabetes shows this is not correct. In a new study published in the July 2016 issue of Pediatric Diabetes, researchers report on a number of studies conducted on deceased children and adults with recently diagnosed diabetes. Because of the wealth of new information in this recently released diabetes report, we'll outline important findings below. Links are active to view the original source. Below are the key points (nearly verbatim) of their paper. Slight modifications in original text were made to make this understandandable to average readers.
| 1 |
BETA CELL LOSS AT 50% - NOT 90%
Previous research [29, 30] and recent findings argue the long held belief that 90% of the beta cell mass is lost at diagnosis is no longer correct. Younger children are expected to have a greater loss, but those diagnosed when teenagers or older were reported to have at least 40–60% of their islets staining positive for insulin [view study1, view study2]. All of these studies were done on recently deceased children and adults with type-1 diabetes through the national program set up in the UK. |
| 2. |
DESTRUCTION OF beta-cells TAKES YEARS
These findings stress autoimmunity is a chronic and ongoing disease, which is present for several years after diagnosis in both children and young adults. All studies appear to agree that insulitis does not affect all islets in the pancreas at the same time, suggesting that this is a process that evolves over time. |
| 3. |
30% OF PANCREAS ISLETS POSITIVE
FOR INSULITIS
Insulitis is when the islets in the pancreas have been infiltrated (attacked) by immune system cells. Overall, the proportion of islets showing insulitis in the human type-1 diabetes pancreas is quite low (∼10–30%); this may vary to some extent by age and disease duration. Insulitis appears more prevalent in younger patients and in those whose pancreas was examined nearer to diagnosis. For example, reports indicate that about 30% of insulin-positive islets are infiltrated in young patients who were recently diagnosed [view study] |
| 4. |
YES! EVEN ADULTS FOUND TO HAVE
INSULIN PRODUCING ISLETS
Six biopsies were performed in adult deceased patients with recent onset type-1 diabetes: insulin staining was found in 18–66% and on average in 36% of the islets examined [view study]. |
| 5. |
BETA-CELLS STILL PRESENT
YEARS LATER
In the analysis of 80 deceased child donors with type-1 diabetes, of whom only a few had disease duration less than 1 yr [view study], residual beta-cells were observed in all child donors with insulitis, who had, on average, a roughly 10-fold higher beta cell mass compared with those without insulitis; there was no correlation of beta cell mass with insulitis, disease duration and age of onset. |
| 6. |
BETA CELL MALFUNCTION (not just loss)
CAUSES TYPE-1 DIABETES
There is increasing evidence that inflammation and beta cell dysfunction (rather than only beta cell loss) may be important mechanisms at the time of initial disease onset and contribute to cause the symptoms of severe hyperglycemia [32-36]. |
| 7. |
EVIDENCE OF BETA CELL HEALING
and
RECOVERY
Moreover, islet function may be recoverable [view study], as shown by the DiViD study: islets isolated from the pancreas obtained via biopsy in newly diagnosed T1D recovered function in culture. This recognition has important implications for the design of therapeutic strategies to reverse diabetes at diagnosis. In fact, the low prevalence of insulitis at diagnosis suggests that even at that time, a therapy that attempts to deplete autoreactive T-cells may only be treating those islets with insulitis, and therefore therapeutic efficacy may be limited. Combination therapies should therefore address pathogenic cofactors, attempt to mitigate inflammation and correct beta cell dysfunction [view study]. |
| |
BETA CELL DESTRUCTION TAKES YEARS
The above findings also suggest that beta cell destruction is quite heterogeneous and is not likely to be completed until several years after diagnosis. Studies have reported persistence of insulin-positive beta-cells even decades after diagnosis [view studies] and that glucose transporters continue to be expressed [21, 41]. |
| |
Beta-Cells STILL PRESENT
YEARS AFTER DIAGNOSIS
Low levels of beta cell apoptosis have been noted in the pancreas of patients with long disease duration, implying the existence of some beta cell turnover [38-40]. |
| |
INSULIN PRODUCTION CONTINUES
YEARS AFTER DIAGNOSIS
Several studies have reported that patients with decades of disease duration may secrete low amount of C-peptide (C-peptide shows insulin is being produced) and also respond with increased levels to stimulation [40, 48-50]. Thus, both pathology data about insulitis and beta cell mass and clinical data suggest that T1D is due to a chronic disease process, which affects islets asynchronously continues its course over a long period of time after diagnosis. |
Pediatric Diabetes
Vol. 17: (Supplement 22): 31-36,
July 2016
Diabetes Research Institute
University of Miami
Miller School of Medicine
Miami, FL USA
Funding by NIH (Natl Institute of Health)
40% Beta-Cell Loss in Diabetes Diagnosis - Not 90%
Early Teen Beta Cell Loss about 60%
In a report to clarify the amount of beta cell loss in people recently diagnosed with type1 diabetes, researchers studied results from 3 separate studies in which scientists counted the number of beta-cells in the pancreas of people who died within one year of diagnosis of type-1 diabetes. This included 106 separate autopsy studies. Results showed that infants with type-1 diabetes have a greater percentage loss in beta cell mass than adults. For example, an 85% reduction in beta cell mass in infants can lead to diabetes, while in early teens this number is about 60% and in adults it appears to be as little as 40%.
In conclusion, the researchers stated,
By re-examining the data obtained from the pancreata of patients who died soon after diagnosis, the extent of beta cell death was found to vary with age, whereby a 40% reduction at 20 years of age is sufficient to precipitate clinical symptoms of type-1 diabetes mellitus. Thus, the statement that an 80–95% reduction in beta cell mass is necessary for the onset of hyperglycemia appeared to be an overestimate for most patients.
PLoS ONE
Vol. 3(1): e1374, 2008
Dept. of Chemical Engineering
Dept. of Microbiology & Immunology
West University, Virginia, UAA
Mayo Clinic College of Medicine, USA
Diabetes 1 in 300 in U.S. by Age 18
Increasing 2-5% worldwide each year
Diabetes Practically Unheard of in 1800's
The 1892 edition of Osler’s Principles and Practice of Medicine devotes 10 pages to diabetes, compared with 65 for tuberculosis, and mentions that only 10 of 35,000 patients treated at Johns Hopkins were affected. Massachusetts General Hospital admitted 47,899 patients over the period 1824–1898, of whom 172 (0.004%) were diagnosed with diabetes.
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
Tasting Urine Main Diagnosis Method in 1850's
Until 1851, diagnosis of diabetes was based on the taste of the urine, which may have limited screening enthusiasm, although the physician in charge “sometimes called upon the house physician to apply this test,” and self-monitoring was occasionally recommended (5). Improved access to urine tests probably accounts for the increased frequency of diagnosis from 1885 onwards, and by 1923, urinary glucose measurement was available in many U.S. drugstores at a cost of 1¢ per test (6).
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
Diabetes Always Fatal to Children Before 1921
Despite reliance on urine tests, the near uniform fatality of childhood-onset cases in series from the preinsulin era testifies that there was little confusion with renal glycosuria. Morse cites Carl von Noorden, the great European authority of the time, who said that “with few exceptions diabetes in childhood knows no cure, no matter how mild it may appear in the beginning, nor how gradual its development in the first months or even years.” His experience was that children under age 7 years with the severe form of the disease survived 18 months to 2 years, while those with “mild glycosuria” lived 3–6 years, and that “the usual statement that the younger the child the shorter the course is true” (7). Joslin reported in 1923 that 86% of children presenting under age 16 years had previously died in ketoacidosis (6).
There is of course no way of knowing how many cases of diabetes had been missed, but one small clue suggests that we should not underestimate the diagnostic skills of our predecessors. A strong family history was already recognized as a favorable prognostic marker, and Joslin remarked that “all cases which have come to my attention of youthful patients with diabetes living for very long periods of time have been hereditary” (6). If Joslin was familiar with maturity-onset diabetes of the young, as Tattersall believed him to be (12), this could provide useful internal evidence that type-1 diabetes was truly rare.
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
How Common was Diabetes Before Insulin?
Insulin was discovered & produced in 1921?
In the absence of epidemiological studies, the only sources available to us are clinic series and mortality statistics. The reported death rate from diabetes for children under 15 years of age was 1.3/100,000/year in the U.S. in 1890, as compared with 3.1/100,000/year in 1920 (6). These results are comparable with those for Denmark, with estimates rounded to 2/100,000/year under age 15 years for 1905–1909 and 4/100,000/year for 1915–1919 (13). Data for Norway can be derived from Gundersen (14) and suggest an incidence rising from 2 to 7/100,000/year over the period 1900–1920. Clinic series are less helpful, since they typically describe the percentage of referrals in each age category. By 1922, Joslin was able to report that 366 (14%) patients in his personal series had been diagnosed in the first two decades of life, with 149 presenting in the first decade. He also comments that the proportion of children in his caseload was rising, although this may have been due to his special interest in the condition, which was readily passed on by other physicians because of the “general feeling of the hopelessness of the disease in children.” Other series quoted by Joslin give a much lower proportion of children under the age of 10 years, ranging from 0.5 to 1.4% of the total, and one Japanese series of 680 patients contained no children at all. His view was that “the increase in the percentage of cases in the first decade as compared with a generation ago speaks emphatically in favor of the better diagnostic methods of today rather than of actual increase in the frequency of the disease” (6), and at this remove of time we must rest content with this conclusion.
We may therefore conclude from this limited evidence that childhood diabetes terminating in ketoacidosis was uncommon but well recognized in the decades before insulin, that mortality statistics show an increasing incidence over the first two decades of the century, probably due to greater awareness of the condition, and that mortality statistics from the U.S., Denmark, and Norway suggest an incidence range of 2–7/100,000/year under age 15 years for the period 1900–1920.
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
Insulin Invented in 1921 - Stops Fatalities from Diabetes
Canadian physician Frederick Banting and medical student Charles H. Best discovered the hormone insulin in pancreatic extracts of dogs. On July 30, 1921, they injected the hormone into a diabetic dog and found that it effectively lowered the dog's blood glucose levels to normal. In fact, Dr. Banting was awarded the Nobel Peace Prize for his accomplishment.
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
Diabetes Still Increasing after 1920
The period between World War I and II saw great advances in public health and the collection of social statistics. A landmark was the U.S. National Health Survey of 1935–1936. This was a doorstep sampling survey of 2.5 million people living in 700,000 households in 83 cities. The reported rate of diabetes for the age-group under 15 years was 0.35/1,000 for boys and 0.41/1,000 for girls (15). For comparison with our other numbers before 1920 this is 35 per 100,000 for boys and 41 per 100,000 for girls. Remember? Back in 1890 it was just over 1 per 100,000 and in 1920 it was up to about 7 per 100,000. In contrast, National Health Interview Surveys undertaken later in the century gave prevalence figures of 1.30 and 1.60/1,000 under age 16 years for 1973 and 1976, respectively, with rates (this time up to age 18 years) of 1.30 for both sexes for 1979–1981 and 1.20 for 1989–1992 (16).
DIABETES
Vol. 51(12): 3353-3361, Dec 2002
Dept. of Diabetes Metabolism
University of Bristol, U.K.
Diabetes Rates in Norway
The main source of incidence and prevalence data for this period is Scandinavia. A Norwegian government survey in 1934, based on a questionnaire to doctors, identified a national total of 253 children under the age of 15 years, giving a minimum prevalence of 0.28/1,000, but ascertainment was undoubtedly incomplete (17). More detailed information about the incidence of diabetes in Norway is available from two retrospective surveys in Oslo and Bergen. Westlund examined all cases of diabetes admitted to hospital in Oslo over the period 1925–1954. His main aim was to document the effect of food rationing during World War II on the incidence of diabetes (Fig. 1), and to do this he needed to establish accurate baseline rates both before and after the war. The assumption was that all cases would be admitted to hospital at diagnosis, and the aim was therefore to identify all first admissions. A total of 4,251 individual patients were identified, and the incidence of diabetes under age 30 years remained relatively constant over the period 1925–1954; the average incidence under the age of 15 years can be estimated as 4.1/100,000/year from the data provided (18).
Meanwhile, an independent Norwegian survey had been conducted in Bergen. This was then a town of some 100,000 inhabitants with one hospital. Per Hanssen made a heroic effort to identify all cases of the disease over the period 1925–1941. Cases were identified by a retrospective search of hospital admissions from 1910 to 1941 and by examination of a city register established in 1940–1941 to ensure that patients with diabetes received food supplements under wartime conditions. In addition to this, a questionnaire was sent to all doctors in the city asking them to register all cases of diabetes prospectively over a 6-month period beginning March 1941, and death certificates and postmortem reports were also checked for the whole period. This exhaustive search identified 402 patients with diabetes alive in 1941, 46% of whom were receiving insulin and a further 392 who had died over the preceding 16 years. The author concluded that the total prevalence of diabetes had doubled over the 15-year period, but this increase was confined to the older age-groups and, as in the U.S. (19), was attributed to the increasing age of the population. A total of 40 individuals developed diabetes under the age of 20 years, equivalent to an incidence rate (based on the 1934 census) of 7.9/100,000/year for this age-group over the period 1925–1939 (17). Although the confidence intervals around such an estimate will be wide, the overall agreement with the Oslo data is good.
The war also had an indirect impact on Sweden, where, based on ration cards issued in 1942, the State Institute of Human Genetics and Race Biology collected national data on the number of people with diabetes in the population. Ascertainment was checked in Stockholm by a survey of patients receiving hospital treatment over the period 1938–1942, and this identified an additional 14% of patients not receiving ration cards. At that time, the city contained 72 diabetic children under 15 years of age, giving a prevalence of just under 1/1,000 (20). The Pediatric Clinic in Vasterbötten in Northern Sweden retrospectively reported a wartime incidence of 10.2/100,000/year. This estimate is the highest available for the period, and it is therefore of interest that Vasterbötten remained a high incidence area, with rates rising to 37.9/100,000/year by 1973–1977 (21).
In summary, studies of the incidence and prevalence of childhood diabetes before 1950 underestimate the true frequency of the condition and must be viewed with caution. Access to medical support was variable, but excellent results were achieved at specialized centers and in regions with good organization of health care. The outlook was not as good elsewhere, and prevalence figures will underestimate the true frequency of the condition. It can however be noted that contemporary estimates from Western countries were generally in good agreement with one another and varied little over the period. The most reliable longitudinal study from Oslo applied the same means of ascertainment over 30 years leading up to 1955 and found little variation in the younger age-groups (18). We therefore need to look later in the century for a major increase in the incidence of childhood diabetes.
|
Lack of Breast Feeding
and Cow's Milk Linked to Diabetes
A number of studies suggest that children who are breast fed for shorter periods of time have higher rates of diabetes. Along with this, research has been conducted which shows evidence of an immune defect in children may be triggered by exposure to a protenin found in cow's milk. This has raised concerns about the recommendation of feeding cow's milk based products to young children. To determine if lack of breast feeding and cow's milk could raise the risk of diabetes, researchers in Canada studied who were breast fed for less than 3 months and reported on their diabetes rates when older. If children were also exposed to cow's milk before 4 months the had a 63% increase risk of diabetes.
Diabetes Care
Vol. 17(1): 13-19, Jan 1994
Dept. of Medicine
McMaster University
Ontario, Canada
The Lancet
Vol. 321(8411): 1083-1086, Nov 1984
Type-1 Diabetes Rising Faster in White Children
The following diabetes study was done with children less than 20 years old.
In 2001, 4,958 of 3.3 million youth were diagnosed with type-1 diabetes for a prevalence of 1.48 per 1000. In 2009, 6,666 of 3.4 million youth were diagnosed with type-1 diabetes for a prevalence of 1.93 per 1000. Looking at all races in 2009, the highest prevalence of type-1 diabetes was 2.55 per 1000 among white youth and the lowest was 0.35 per 1000 in American Indian youth. This means that white children had 8 times more diabetes than American Indian children of the same age. Adjusted for completeness of ascertainment, there was a 21.1% increase in type-1 diabetes over 8 years. In looking at type 2 diabetes - In 2001, 588 of 1.7 million youth were diagnosed with type 2 diabetes for a prevalence of 0.34 per 1000. In 2009, 819 of 1.8 million were diagnosed with type 2 diabetes for a prevalence of 0.46 per 1000. In 2009, the number of children with type 2 diabetes was 1.20 per 1000 among American Indian youth - 1.06 per 1000 among black youth - 0.79 per 1000 among Hispanic youth and 0.17 per 1000 among white youth. After adjustments, a 30.5% overall increase in type 2 diabetes over the 8 year period. In conclusion, these numbers show a rapidly expanding rate of type-1 diabetes in young white children and a rapidly expanding rate of type 2 diabetes in children of other races.
Living Longer Not a Reason
for Worsening Diabetes - Here's Why...
You'll hear two main reasons why people think diabetes is worsening; One is obesity, and the other is simply that people are living longer. Under first examination, this makes sense since diabetes rates do increase as people become older - well almost... except for one very, very important fact - People born before World War II (who were over age 70 at the time of the study) had a 5 percentage point lower rate of diabetes than people age 60-69. Think about this - people who were 71, 75, 80 and 85 had a 63.8% diabetes rate and people age 60-69 had a 68.6% diabetes rate. Fascinating isn't it. So, there is something unique about people born before World War II. Explainations for this will be discussed later and This fact, shows it is more than just age. First, the percent of people with diabetes in every age group is increasing - not just the total numbers. Therefore, when looking at the "percent of a population" with diabetes, it doesn't matter if more people are living longer and more are being counted since we are only concerned with the percent of people affected and not total numbers. It doesn't matter if you are investigating diabetes in 1 million or 100 million people over the age of 60, the percent of the total group is the only number that will tell us if diabetes is worsening. Another very important point, the percentage of children under age 5 with diabetes is increasing even faster than all diabetes in the adult population. This is also true for type 2 diabetes in children ages 10 to 19. In this current study out of Saudi Arabia investigating diabetes rates in different age groups, it was found that people over 70 years of age had lower rates of diabetes than those in the younger age groups. This was a surprising find and leads to speculation on why this might be happening. Below are the rates of diabetes in the different age groups as reported in this 2011 study published in the Annals of Saudi Medicine. People age 60-69 had a diabetes rate of 68.6% while people over 70 had diabetes rates of only 63.8%. Why the nearly 5 percentage pont drop for the oldest population?
| Age 12-19 |
2.0% |
| Age 20-29 |
4.6% |
| Age 30-39 |
12.1% |
| Age 40-49 |
31.9% |
| Age 50-59 |
58.2% |
| Age 60-69 |
68.6% |
| Over 70 |
63.8% |
CHEM-TOX COMMENT: This finding showing the oldest members of society (those born before 1945) had a lower rate of diabetes than the younger group strongly supports the conclusion that something was quite different for the older group at some point in their lives. Factors to consider include such things as - those born before 1945 had lower exposure to petroleum chemiclas used in consumer products, pesticides and vehicle exhaust (as these exposures increased exponentially after World War II). Therefore, the assumption can be made that the oldest people in society were exposed to far less chemicals during while developing in the womb during their mother's pregnancy. This leads to the postulation that increased chemical exposure could have a negative effect on beta-cell growth and maturation during pregnancy and the first few years of life. This also raises the question on whether children today have different numbers of beta-cells at birth, which could potentially lead to earlier onsent of diabetes for those with low beta cell numbers at birth.
Beta Cell Loss Occurs in 3 Stages
Scientists believe diabetes occurs in 3 stages: First, beta-cells in the pancreas are damaged or destroyed by various processes including autoimmune in type-1 and unknown in type 2. Next, malfunction of glucose control when insulin is sufficiently impaired causing liver insulin resistance. In the final stage, glucose toxicity occurs in which higher blood sugar levels accelerate damage and dysfunction among remaining beta-cells.
Autopsy Study: Total Beta-Cells Differ Dramatically
in Children without Diabetes
Evidence why some more likely to develop diabetes
Islets are like small "islands" in the pancreas that contain beta-cells. On average, the findings in this study show a typical islet contains a little more than 1000 beta-cells. This study shows that while the number of islets is relatively stable from birth, the number of beta-cells within the islets continues to increase until about age 5. The total number of islets in the human pancreas differs dramatically from one person to the next. In this study of 46 deceased children whose parents donated their children's pancreas for investigation (ages 2 weeks to 21 years), there was more than a 10-fold difference between the lowest and highest number of islets. The chart at left shows the number of islets in millions (left vertical line) and ages of children along the bottom horizontal line. While most organs within the body show similar numbers of cells from person to person, the number of islet containing beta-cells varies dramatically from child to child. For example, when looking at the cluster of 14 children less than 3 years old, 1 child had about 3 million islets - 1 child about 2 million islets - 3 children had about 1.5 million - another 3 children had about 1 million islets and 4 children had from about 400,000 to 700,000 islets. The researchers commented that this discrepancy between children is of concern as children starting life with a "low" number of islets (and therefore beta-cells) would be more likely to develop diabetes at a younger age than others with higher islet numbers. Another finding of this study was that while the number of islets remains about the same in a child from birth to age 5, the actual number of beta-cells within the islets increases markedly in number and size as the child grows up until age 5.
CHEM-TOX COMMENT: As the difference in total number of islets between these children is so dramatic, it suggests that enviromental rather than genetic factors may be responsible for suppression of islet and beta cell growth during pregnancy. This observation provides a logical reason on why type-1 diabetes may be growing so rapidly in young children under age 5. Future studies need to be done with experimental animals to determine differences in islet growth depending on various environmental exposures during pregnancy. For example, do pregnant rats exposed to low levels of pesticides or phthalates etc., have offspring with lower numbers of islet cells at birth?
DIABETES
Vol. 57(6): 1584-1594, June 2008
Larry Hillblom Islet Research Center
Division of Endcrinology
UCLA David Geffen School of Medicine
Los Angeles, California, USA
Beta-Cells Begin Forming at 9 Weeks into Pregnancy
As the previous study shows dramatic differences in the total number of islets and beta-cells in deceased children, it is important to find out when beta-cells form during pregnancy to help in future research to determine why this might be happening. To answer this question, scientists examined 65 human embryos and fetuses from 8 weeks after conception onward. Tissue samples were from miscarriages and legal abortions in Germany. The chart at right shows the percent of recent beta cell division in comparison to the age of tissue sample. undergone replication. The left vertical line represents the percent of beta-cells that recently divided and bottom line represents the time in gestational weeks. As can be seen, beta-cells began forming at about 9 weeks into pregnancy and continued basically throughout the entire pregnancy.
European Journal of Endocrinology
Vol. 162: 559-568, March 2012
Department of Medicine
Ruhr-University of Bochum, Germany
Department of Anatomy
Medical University of Innsbruck, Austria
Evidence Adult Beta-Cells Regenerate
Researchers analyzed the pancreas' from 9 deceased adult donors. Researchers found that 15% of all beta-cells were found in units with a diameter less than 20 microm and in the same areas of the pancreas that "budding" (growing) beta-cells are found in fetal and neonatal organs. Having beta-cells of smaller size along with being located in specific areas of the pancreas led researchers to state the following:
The high proportion of budding beta-cells in the adult human pancreas suggests the presence of numerous loci with a potential for beta cell neogenesis (Neogenisis is the terminology for "new beta cell growth").
For a full review of research on beta cell regeneration in animals and humans see the study entitled NeogenChildrenesis: A Possible Pathway for Beta-Cell Replenishment (Reviews in Diabetes Studies, 9(4): 407-416, 2012)
Diabetologia
Vol. 41(6): 629-633, June 1998
Diabetes Research Center
Free University of Brussels, Belgium
Prediabetes Predicts 75% Chance of Diabetes in 10 Years
As of 2012, the rates for combined diagnosed and undiagnosed adult diabetes was between 12%- 14% in the United States. Prediabetes (as defined by a fasting blood glucose level of 100-125) was estimated to be 35-39% in the U.S. population. According to the American Diabetes Association, as quoted in this current study - 75% of people with prediabetes develop diabetes within 10 years. This means that another 25% of the population with join the existing 14% with diabetes for a total of over 35% with diabetes by 2022 (taking into consideration there will be some deaths in the current 14% with diabetes).
CHEM-TOX COMMENT: As 35% of the U.S. population had prediabetes as of 2014, we can then accurately preduct that 75% of this group will have full-blown diabetes in 10 years. This works out to nearly an additional 25% of the U.S. population being diagnosed with diabetes in 10 years. Combine this with the current 12% diabetes rate in 2014, we can then expect to have over 35% of the U.S. population to have diabetes by 2014 (12% plus 25%) and over 50% of the population with diabetes within another 10-15 years after that.
LANCET
Vol. 379(9833): 2279-2290, Jan 2012
Adam G Tabak, MD, PhD
Dept. of Epidemiology & Public Health
University College London, UK
Higher Cancer Rates for People with Diabetes
Is it the Diabetes or Insulin?
While its openly discussed that people with diabetes have higher rates of diseases affecting the kidneys and vision, it is much less known that people with diabetes have higher rates of some cancers. For example, as reported in the introduction of the journal Diabetologia, studies have shown that people with diabetes had a 30% higher rate of colorectal cancer - a 24% higher bladder cancer - and a 20% higher rates of breast cancer. To address this growing health problem, the American Diabetes Association and American Cancer Society came together to hold a conference in December of 2009. As stated in their report, diabetes has been shown to nearly double the risk for cancers of the liver, pancreas and endometrium and increases the risk for cancers of the colon, rectum, breast and bladder by 20-50%. Along with increased risk of these cancers, some studies show that once cancer is diagnosed, people with diabetes have considerably less chance of surviving 5 years than those who do not have diabetes. For example, in one study, 5-year death rates were about 40% higher in diabetes patients diagnosed with both breast cancer than comparable breast cancer patients without diabetes (see study). This report also stated that something besides high blood sugar is driving the higher cancer rates as studies of type-1 diabetes do not find high blood sugar increases cancer growth (see study).
CHEM-TOX COMMENT: It's interesting to note that diabetics have been found to be less likely to survive 5 years after cancer diagnosis. Other studies on other populations shows people with lower levels of lymphoctyes (which include natural killer cells) are less likely to experience remission from cancer. Also, recent studies show that patients with type 2 diabetes often have a combination of type-1 as well, thereby suggesting an autoimmune intereaction is possible which could increase soft tissue damage in various organs, thereby increasing cancer risk as well.
Diabetes Care
Vol 33(7): 1674-1685, July 2010
Dept. of Epidemiology
Harvard School of Public Health
Boston, Massachusetts, USG
Insulin Appears to Increase Cancer Risk
It is well documented that people with diabetes have significantly higher rates of cancer than the general population. To investigate if taking insulin could be involved with this increased risk, researchers in Germany studied 127,031 diabetic patients taking different types of insulin and followed their medical history for up to 4.4 years. Patient groups included those treated exclusively with either human insulin, aspart insulin, lispro insuline or glargine insuline (Lantus). Unlike other similar studies, patients involved in this study were taking only one type of insulin. Results showed there was no increased risk of cancer for those taking aspart or lispro insulin compared with human insulin. However, a dose dependent increased risk of cancer was found for those using glargine insulin (Lantus). For example, those taking a daily dose of 10 IU of Lantus had approximately 10% increased risk of cancer - those taking 30 IU had a 19% increased risk of cancer - those taking 50 IU had a 31% increased risk of cancer. In conclusion, the researchers stated,
Considering the overall relationship between insulin dose and cancer, and the lower dose with glargine [Lantus], the cancer incidence with glargine was higher than expected compared with human insulin. Our results based on observational data support safety concerns surrounding the mitogenic properties of glargine in diabetic patients. Prospective long-term studies are needed to further evaluate the safety of insulin analogues, especially glargine.
Diabetologia
Vol 52(9): 1732-1744, Sep 2009
Hanover Medical School, German
University of Cologne, Germany
Problems with Chemical Based Insulin:
Increases Colon & Rectal Cancer in Diabetics
This study was conducted to determine if insulin therapy would increase the risk of colorectal cancer among people with type 2 diabetics. All type 2 diabetic patients in the General Practice Research Database from the United Kingdom were included in the study. This included 3,160 patients using insulin and 21,758 patients not using insulin. Results showed that those not using insulin had a colorectal cancer rate of 124 per 100,000 years while those using insulin had a colorectal cancer rate of 197 per 100,000 person years. Initially, this shows over a 50% increase rate of cancer for those taking insulin. After adjusting for age, sex and other factors, the postive association strengthened further suggesting nearly twice the risk of developing colorectal cancer. A dose-response effect was also seen resultig in a higher cancer rate for each year of insulin use. In conclusion, the researchers stated,
"Chronic insulin therapy significantly increases the risk of colorectal cancer among type 2 diabetes mellitus patients."
Gastroenterology
Vol. 127(4): 1044-50, Oct 2004
Division of Gastroenterology
Univ. of Pennsylvania School of Medicine
Philadelphia, USA
Some Antibiotics May Lead to Severe Blood Sugar Swings
To determine if antibiotic use could affect blood sugar levels, researchers investigated antibiotic use and hospitalizations among 78,000 people with diabetes in Taiwan. Antibiotic categories included the three classes: fluoroquinolones, cephalosporins and macrolides. Doctors then looked at emergency room visits and hospitalizations for severe blood sugar swings among the patients in the 30 days after they started taking antibiotics. The rate of severely high blood sugar was about 7.0 per 1,000 for people taking the antibiotic moxifloxacin, 3.9 for levofloxacin and 4.0 for ciprofloxacin. Rates were only 1.6 for those taking macrolide antibiotics and 2.1 for cephalosporins. Very low blood sugar was also found to occur - patients taking moxifloxacin had a rate of 10 per 1000. In conclusion the researchers stated,
"Diabetics using oral fluoroquinolones faced greater risk of severe dysglycemia. The risk of hypoglycemia varied according to the type of fluoroquinolone administered, and was most commonly associated with moxifloxacin."
Living Near Toxic Waste Sites Increase Risk of Diabetes
In this study done by the University of Albany, New York, researchers investgated diabetes rates for people living near toxic waste sites in New York and along the Hudson River. Toxic waste sites expose people living in the area to higher levels of chemicals either through evaporation into the air or through leaching into ground water and subsequent drinking of the water. All hospitals in the state of New York are required by law to report every diagnosis of diabetes upon discharge. To increase accuracy of results, reseachers reported only on Caucasians and African Americans with incomes between $31,107 and $51,482. Hazardous waste sites were identified in New York from information from the U.S. EPA and New York State Department of Environmental Conservation. A total of 818 sites (and Superfund sites) were identified as a potential threat to human health. Researchers then took the zip codes people diagnosed with diabetes and matched these to zip codes of toxic waste site. Compared to people living in clean zip code areas, people living closer to Toxic Waste Sites had an overall 23% increase rate of diabetes rates. For people living near toxic waste sites along the Hudson River had a 36% increased rate of diabetes. Chemicals frequently emitted from toxic waste sites include PCBs and dioxin, both of which have been shown to increase risk of diabetes.
Adding Fluoride to Water Increases Rate of Diabetes
Researchers hypothesized that water fluoridation was contributing to the quadrupling of diabetes over the past 32 years in the United States. Fluoride is sometimes found naturally in groundwater in the form of calcium fluoride, however, the type added to city water supplies comes in the form of fluorosilicic acid and sodium fluorosilicate and sodium fluoride. Fluorosilicic aced is the type formed as a by-product of making chemical fertilizers. To test their diabetes/fluoride theory, researchers measured levels of natural and added fluoride to water supplies in counties across 22 states in the U.S. Their study also took into account the amount of water used in the counties as well. Results showed that a 1mg increase in the county fluoride level significantly predicts a 0.23 per 1000 person increase in age-adjusted diabetes incidence and a 0.17% increase in the percent of people with diabetes. In conclusion, the researchers stated, "Community water fluoridation is associated with epidemiological outcomes for diabetes."
Journal of Water & Health
Vol. 14(5): 864-877, October 2016
Inst. of Health & Eviron Research, Ohio
Dept of Epidemiology & Biostatistics
Case Western Reserve University
School of Medicine
Cleveland, OH, USA
Fluoride Reduces Insulin Production
Researchers administered fluoride to both animals and humans in this study to investigate changees in glucose and insuliln production. Rats were given a single dose of 0.5 ml/100 grams body weight of a sodium fluoride solution through an inserted gastric tube. Glucose tolerance tests were carried out.
Calcified Tissue International
Vol. 46: 330-338, 1990
Evidence Glucose Metabolism Affected by Fluoride
Forty 7 week old male rats were given a single injection of sodium fluoride and compared to a control group of rats not given sodium fluoride. Over the next 30 minutes - glucose levels were measured. Results showed that rats receiving fluoride had significantly higher glucose levels of approximately 115 mg/dl compared to approximately non-fluoride rats whose gluocse levels were approximately 85. This study can be seen HERE. In this next study done in Argentina, researchers give a single sodium fluoride dose of While the previous study mesured glucose levels from a single dose of sodium fluoride, this next study investigated glucose levels after continuous daily oral administration of sodium fluoride and monofluorophosphate over 3 months.
Study #1
Study #2
Study #3
Food Additive MSG Decreases Beta Cell Mass
MSG is the abbreviation for the food additive Monosodium Glutamate. It is added to foods to increase their "flavor profile" - thereby giving the impression of improved taste of many foods including seafood, meats, Chinese food and many salt based snacks. Its use has been increasing in parallel with the epidemic of metabolic syndrome. The authors in this current study stated in their introduction that previous studies have shown MSG given to rodents increases obesity, hyperglycemia, insulin resistance and type 2 diabetes, although the impact of dietary MSG is still being debated. To test the effects of long term use of MSG, 80 adult rats were divided into 4 groups. Each group was then divided into 2 smaller groups, one would receive MSG in its drinking water and the other group would not. Each group was then followed from 1 to 9 months and sacrificed and examined. Results showed that MSG treated rats had significantly lower beta cell mass at 1 month, 3 months and 9 months than non-MSG animals. Studies of islets (which hold beta-cells in the pancreas) showed that the amount of hemorrhages increased with age in all groups and fibrosis was significantly more frequent in MSG treated rats at 1 month and 3 months. Interestingly, insulin levels and glucose tolerance in MSG treated and untreated rats were similar, thereby implying that damage is ongoing from MSG but may take a longer time to see the effects.
PLoS One
Vol. 10(6): e0131595, Jun 29, 2015
Dept of Biochemistry
Khon Kaen University, Thailand
Humanitas Clinical & Res Center, Italy
University of California, Davis, USA
Higher Obesity and Metabolilc Syndrome
in Families Using Monosodium Glutamate (MSG)
Researchers found that healthy volunteers eating MSG with their meals had higher rates of obesity and metabolic conditions associated with diabetes. In this study, conducted in Thailand, 324 families with 487 individuals volunteered to use MSG with meals and keep detailed records of MSG use. Participants had physical examinations for body weight, waist circumference and blood tests. MSG intake ranged from .4 to 14.0 grams per day for the those completing the study. People were then divided into 3 groups (from low to high) according to the amount of MSG consumed. After comparing results between the 3 groups, researchers said they found a significant association between the risk of metabolic syndrom and MSG daily consumption. The prevalence of metabolic syndrome and being overweight was significantly higher in the group with the highest MSG intake. Results showed that every 1 g increase in MSG intake significantly increased the risk of metabolic syndrome by 14% and/or being overweight by 16%. This was independent of total energy intake and the level of physical activity.
CHEM-TOX COMMENT: It is interesting to point out that increases of the health problems discussed was compared among all families using MSG daily. It would be interesting to do a comparison between families using high amounts of MSG and those using none at all. This could potentially lead to even greater differences in results.
Researcher Recommends Banning MSG
Induces Obesity and Inflammation in 12 Month Study
Authors stated in their summary that they have previously reported that MSG was found to lead to central obesity and type 2 diabetes in mice. In this current study, researchers found that mice exposed for 6 to 12 months to MSG resulted in damage to the liver along with evidence of precancerous lesions. Results also showed significantly increased obesity and diabetes. In conclusion the researchers stated:
These results take on considerable significance in light of the widespread usage of dietary MSG and we suggest that MSG should have its safety profile re-examined and be potentially withdrawn from the food chain.
Fluoride Diabetes Review
In a report by Dr. Geoff Pain (Ph.D), he cited a number of studies linking fluoride in drinking water with diabetes. Below is a summary of the studies he referenced:
| Fluoride reduces insulin production in rats |
Lin 1976 |
| Blood fluoride levels of just 234 ppb after a single acute dose caused significant impairment in glucose metabolism, as evident by a sharp rise in blood glucose and decreases in insulin. |
Whitford 1987 |
| Similar results have been measured in rats and human volunteers. |
Rigalli 1990
Suketa 1985 |
| Insulin resistance in humans caused by chronic fluoride exposure from drinking water is well known. |
Bergman 2013
VAndenberg 2012
Chiba 2012
Menoya 2008
Stephen 1994
TRivedi 1993 |
| In chronic exposures to fluoride, effects on glucose metabolism occurred when plasma fluoride concentrations exceeded 0.1 mg/L (5 Umol?L) or just one 15th the concetnration allowed in Austrailian drinking water. |
Rigali 1992, 1995
|
| The U.S. National Research Council 2006) stated, "In general, impaired glucose metabolism appears to be associated with serum or plasma fluoride concentrations of about 0.1 mg/L or greater in both animals and humans. |
|
| Townsville in the state of Queensland, Australia, fluoridated since 1964, suffers 10% higher rate of diabetes than the rest of non-fluoridated Queensland. Townsville also suffers higher rates of hospital admissions for unspecified dental conditions as well as asthma, congestive heart failure, convulsions and epilepsy, congestive obstructive pulmonary disease, ear nose and throat conditions and pyelonephritis. Townsville also suffers increased death rates due to circulatory system, ischaemic heart disease, cerebrovascular disease – Stroke, chronic lower respiratory disease and cancer of the trachea [Queensland Hospital Data 2005-2006]. Townsville can therefore be considered a randomised control trial centre for Fluoride toxicology. |
[PHIDU 2005] |
| Workers in the phosphate fertilizer industry are exposed to fluoride and experience higher incidence of diabetes as well as skeletal fluorosis. |
[Renke 1987] |
| Workers in the cryolite industry also suffer Chronic Fluoride Intoxication (CFI) and have lower insulin and increased C-peptide serum levels. It was shown that the incidence of diabetes increased with years of exposure. |
[Tokar 1992] |
| Insulin secretion (both basal and glucosestimulated) by isolated islets of Langerhans in vitro is inhibited as a function of fluoride concentrations. |
[Rigalli et al. 1990, 1995]. |
Fluoride Causes Diabetes
Technical Report - 2015
Geoff Pain (Ph.D)
Analytical Chemistry
Atmospheric Chemistry
Biochemistry
Insulin Resistance Higher
from Consumer Products Containing 3 Chemicals
Researchers studied 110 male workers who worked around 3 chemicals known as monocyclic aromatic hydrocarbons (called MAHs). This inlcudes the chemcals styrene, toluene and xylene. These chemicals are frequently used in industry. For example, the chemical styrene is used to make fiberglass boats, surfboards, and many plastics. It is also found in car exhaust - in print shops and in styrene-butadiene rubber products in carpeting and auto tires. Many consumer products contain styrene including shoes, food containers, floor tiles, polishes, adhesives, putties and varnishes (see research). People are exposed to toluene by breathing car exhaust, pumping gasoline, using lawn mowers and weed eaters, in kerosene lamps and paints. Fingernalil polish also contains high levels of toluene and is often applied in areas of low ventilation in homes and bedrooms, thereby concentrating the chemical. One large source of styrene would be in homes and apartments with carpet flooring and is of concern because of the reduced ventilation and continuous exposure. Since these chemicals are used throughout society, researchers wanted to determine if they could increase health problems associated with diabetes. Researchers compared 110 male workers who worked around these chemicals with 110 age-matched male workers who had not been exposed to major sources of organic solvents. Results showed that total cholesterol, fasting glucose, fasting insulin, and homeostasis model assessment of insulin resistance levels were significantly higher in those exposed to the chemicals. In conclusion the reseachers stated,
This study indicated that MAHs (the 3 chemicals) increase fasting glucose level and insulin resistance. Furthermore, these results suggested that absorbing the organic solvent itself and active metabolic intermediates can increase oxidative stress and cytokine levels, resulting in the changes in glucose metabolism and the induction of insulin resistance.
Safety Health Work
Vol. 2(4): 365-74, Dec 2011
Occup. Safety & Health Res. Institute
Korea Occup. Safety & Health Agency
Incheon, Korea
Carpets In Apartments & Homes
Emit Chemicals Linked to Diabetes
Anyone who has entered a home or apartment with carpets less than 3-6 months old will often bit hit by a very strong unique chemical odor. This odor is courtesy of dozens of different chemicals that evaporate into the air from carpeting and carpet backing. Unlike wool carpets of many decades ago, modern carpets are made from dozens of petroleum based chemicals. The backing that holds the fibers can be made from the chemicals styrene, butadiene and many other chemicals including one known as 4-Phenylcyclohexene (which we'll call 4-PCH from here on). According to a 2002 report from the National Institute of Environmental Health Sciences in Research Triangle Park, North Carolina, 4-PCH is one of the 12 most frequently found chemicals entering the air from carpets with styrene-butadiene rubber backing. These chemicals are considered volatile, meaning they evaporate into the enclosed air space easily. For example, air concentrations measured in buildings after new carpet installation ranged from 0.3 to 2.6 parts per billion (2ug/m3 to 17 ug/m3).
A CHEMICAL FACTORY
Not only do carpets emit dozens of chemicals into the indoor air, but a number of these chemicals react with ozone to form new toxic chemicals. Ozone itself forms from car exhaust so is constantly around us. Researchers found that 4-PCH and other carpet chemicals react with ozone at levels often found in indoor air to produce formaldehyde and other chemicals known as aldehydes.
As we reported earlier that styrene has been linked with diabetes and that formaldehyde results in antibodies that can increase diabetes, anyone or wishes to decrease their risk of diabetes or worsening the condition should certainly avoid new carpeting if possible.
Gasoline Additive Linked to Higher Fasting Glucose
The chemical known as MTBE is added to gasoline as an octane booster and to increase oxygen in gasoline used in gasoline engines. People breathe this chemical daily while filling their gas tank and while driving in traffic. Researchers hypothesized that MTBE could hinder zinc and normal glucose levels in rats. To test this theory, 42 male rats were divided into seven groups with 6 rats per group. Groups were exposed to different levels of MTBE and groups 6 and 7 also received zinc acetate. Animals received MTBE in drinking water for a total of 90 days. At the end of treatment their pancreas and blood samples were collected for examination. Results showed that animals exposed to MTBE had a significant increase in fasting blood glucose and total cholesterol which was observed in a dose-dependent manner. It also increased C-reactive protein, which is evidence of inflammation and autoimmunity. MTBE was also found to significantly decrease zinc levels. Zinc is an essential element required for maintatining normal glucose levels. It has also been reported that low serum zinc concentrations are evident in the early phases of type-1 diabetes.
Xenobiotica
Vol. 1-6, July 7, 2016
Dept. of Pharmacology & Toxicology
University of Medical Sciences, Iran
Evidence Humans Do in Fact Grow New Beta-Cells
but is Highly Affected by Glucose Levels and Age
In the scientific community, it is well known that animals have the ability to regenerate new pancreatic beta-cells, but this also depends on age. For example, while young rats can grow beta-cells at a relatively fast pace (as seen after intentional damage to the pancreas), the rate decreases to about 1-3% per day in older rats. Although beta-cell growth is believed to also occur in humans, the extent of this regeneration is not well understood and can be reduced (or eliminated) if autoimmune cells or high blood glucose levels (called glucose toxicity) destroy immature beta-cells "trying to grow" in the pancreas. To determine if and how well humans can grow new beta-cells, scientists measured the growth (and death) of cultured human beta-cells under different glucose concentrations from 53 organ donors ranging in age from 17 to 74 years. In both older rats and humans, increasing glucose from 100 mg/dl (5.5 mmol/l) to 600 mg/dl (33.3 mmol/l) resulted in a linear increase in beta-cell death and large reduction in proliferation. Age was also a major factor as beta-cells from older donors died in far less time at higher glucose levels.
DIABETES (J from Am. Diab. Assoc)
Vol. 55(9), 2455-2462, Sept 2006
Marc Y. Donath, MD
Division of Endocrinology & Diabetes
Dept. of Medicine
University Hospital
Zurich, Switzerland
Beta-Cells Replenish
and Grow in Adult Lewis Rats
As people with type-1 diabetes (and now type 2) have lower numbers of beta-cells in their pancreas, it is important to determine to what extent humans can regenerate lost or damaged beta-cells that produce insulin. Scientists at the University of Barcelona set out to determine how fast beta-cells reproduced - how many beta-cells were destroyed and the beta-cell mass in Lewis rats at different times throughout their lifespan. Lewis rats can often live up to 24 months. They divided rats into different groups and performed humane killings and subsequent pancreas analysis at 1 month - 3 months - 7 months - 10 months - 15 months and 20 months. Results showed beta-cell mass increased 8 times from 1 month to 20 months (typically a very old rat). The number of beta-cells per pancreas also tripled from month 1 to month 7. In their "DISCUSSION" - scientists stated that this is the first study to show that beta-cell growth is maintained throughout the entire lifespan in normal rats and that beta-cell growth remains stable after young adulthood, clearly establishing that beta-cell birth rate does not fall to 0, even in late periods of life.
Diabetes -
Full PDF
Vol. 49(8): 1341-1346, Aug 2000
Laboratory of Diabetes & Exp Encocrin
University of Barcelona, Spain
Astounding 50x's higher Autoimmunity
for Type 2 Diabetics with Neuropathy
There are many health disorders that occur with far greater freuquency among people with diabetes. Neuropathy is one of these. Neuropathy is simply a disease in which nerves in different parts of the body lose their ability to function properly. Nerves control eye movement, muscle movement and even your heartbeat, thereby showing that many bodily functions can be damaged by neuropahty. This diabeteic nerve damage occurs when the tiny blood vessels carrying blood to the nerves shrink in size, resulting in less blood and nutrients reaching the nerves. If nerves don't get enough blood, they begin to malfunction and die. Longer nerves such as those to the feet are apparently more vulnerable to this type of damage which explains why foot and leg amputations are more common among diabetics. The reduced blood flow occurs as the tiny blood vessels decrease in diameter.
To determine if blood vessel damage occurs because of autoimmunity, investigators in Scotland studied blood samples from 30 diabetic patients with neuropathy - 30 diabetic patients without neuropathy and 30 healthy control subjects. Blood samples were measured for what are called antinuclear antibodies. Antinuclear antibodies bind to the cell nucleus, and serve as a signal to be attacked by other immune system white blood cells. Results showed that people with diabetic neuropathy had an astounding 50 times greater number of antinuclear antibodies than the healthy control group. A secondary analysis found a dose-response connection showing that as levels of antinuclear antibodies increased - there was an associated worsening of neuropathy. In conclusion the researchers stated,
The study demonstrated for the first time that human peripheral diabetic neuropathy may have an autoimmune aetiology.
Immunology Letters
Vol. 168(1): 73-9, Nov 2015
Queen Margaret University, Scotland
Dept of Podiatry
Bahrain Defense Force Hospital
Artificial Sweetener
Increases Diabetes Symptoms
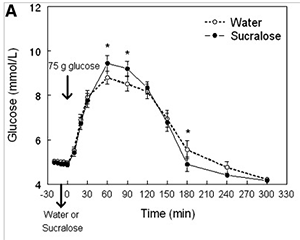 Studies on artificial sweeteners are a bit tricky. While some show problems with worsening glucose or diabetes symptoms - others do not. For example, in a study reported in the October 2017 journal Nutrition and Metabolism, researchers had 31 adults drink Diet Mountain Due and Diet Rite Cola to investigate effects on glucose blood levels and other diabetes related symptoms. The good news was there were no major effects seen on glucose although increases in insulin were observed (which is peculiar since no carbohydrates were in the drinks). However, when looking closer at the study design we see the 31 individuals chosen to participate in the study were all "healthy adults" without any signs of diabetes or obesity. Since sugar-free products are typically used by people who are either overweight or diabetic, it would have been more enlightening to also have conducted the study with people who were in fact obese and/or diabetic. In an attempt to do just this, a similar study was conducted by Dr. Yanina Pepino and colleagues at the Center for Human Nutrition at Washington University School of Medicine. Here, they acquired the assistance of 17 obese subjects (15 African American and 4 Caucasian) who were not diabetic but did show very marginal signs of being insulin sensitive (getting close to type-2 diabetes). So, here, they weren't completely healthy or fully diabetic, but just like Goldilocks and the 3 Bears - they were just right for the study as they would typically be the type of person who would use artificial sweeteners. Also, to be included in the study, they could not have consumed more than 1 diet drink or one spoonful of diet sugar per week in the preceding weeks. Now getting back to our study - each of these 17 brave souls were held captive in a chair for 5 hours with a needle in their arm while they were measured for glucose changes in their blood after consuming two different drinks. To begin, some were given the equivalent of a 12-oz sucralose (splenda) diet soda and others drank an equal amount of water. Meausrements of glucose were taken over several hours and the each was give their other drink. The study was then repeated again on a different day but with the other drink. Results showed that after consuming the artificial sugar sucralose drink, each person had significantly higher blood glucose than those drikng water. There was also an increase in insulin and C-peptide (a sign of insulin production).
Studies on artificial sweeteners are a bit tricky. While some show problems with worsening glucose or diabetes symptoms - others do not. For example, in a study reported in the October 2017 journal Nutrition and Metabolism, researchers had 31 adults drink Diet Mountain Due and Diet Rite Cola to investigate effects on glucose blood levels and other diabetes related symptoms. The good news was there were no major effects seen on glucose although increases in insulin were observed (which is peculiar since no carbohydrates were in the drinks). However, when looking closer at the study design we see the 31 individuals chosen to participate in the study were all "healthy adults" without any signs of diabetes or obesity. Since sugar-free products are typically used by people who are either overweight or diabetic, it would have been more enlightening to also have conducted the study with people who were in fact obese and/or diabetic. In an attempt to do just this, a similar study was conducted by Dr. Yanina Pepino and colleagues at the Center for Human Nutrition at Washington University School of Medicine. Here, they acquired the assistance of 17 obese subjects (15 African American and 4 Caucasian) who were not diabetic but did show very marginal signs of being insulin sensitive (getting close to type-2 diabetes). So, here, they weren't completely healthy or fully diabetic, but just like Goldilocks and the 3 Bears - they were just right for the study as they would typically be the type of person who would use artificial sweeteners. Also, to be included in the study, they could not have consumed more than 1 diet drink or one spoonful of diet sugar per week in the preceding weeks. Now getting back to our study - each of these 17 brave souls were held captive in a chair for 5 hours with a needle in their arm while they were measured for glucose changes in their blood after consuming two different drinks. To begin, some were given the equivalent of a 12-oz sucralose (splenda) diet soda and others drank an equal amount of water. Meausrements of glucose were taken over several hours and the each was give their other drink. The study was then repeated again on a different day but with the other drink. Results showed that after consuming the artificial sugar sucralose drink, each person had significantly higher blood glucose than those drikng water. There was also an increase in insulin and C-peptide (a sign of insulin production).
The results from the current study demonstrate that the ingestion of sucralose alters the metabolic response to an oral glucose load in obese people who are not regular consumers of Non-Nutritive Sweeteners. The peak increase plasma glucose, C-peptide, and insulin concentrations and total insulin AUC after an oral glucose load were greater when subjects consumed sucralose than when they consumed water before glucose ingestion.... In addition, insulin clearance from plasma was slower after sucralose than after water ingestion. These data suggest that sucralose ingestion is not physiologically inert but affects the glycemic response to an oral glucose load and potentiates glucose-stimulated insulin secretion in obese people.
Diabetes Care
Vol. 36(9): 2530-2535
August, 2013
Dr. Yanina Pepino, PHD
Center for Human Nutrition
Washington University School of Medicine
St. Louis, Missouri, USA
Artificial Sweetened Drinks Double Rates of Obesity
While not specifically linked to diabetes directly, this study is being included as obesity is often discussed as a risk factor for diabetes. Many people consume artificially sweetened drinks believing it will help them lose weight. However, this study shows the opposite may be occurring. Instead of using sugar, diet drinks are sweetened with chemicals such as aspartame and sucralose. To determine if chemical based sugars were helping people lose weight, researchers studied 5,158 adult residents of San Antonio, Texas from 1979 to 1988. All participants were measured for height - weight and artificial sugar consumption at the beginning of the study. Seven to eight years later, 3,682 survivors were re-examined. Results showed that as the number of diet drinks increased, there was a corresponding increase in weight gain, obesity and BMI. A BMI of 25 is the cut-off for being overweight and a BMI of 30 is the cut-off for being obese. For example, when looking at the 1,250 people who were normal weight at the beginning of the study, those drinking 1 or 2 diet drinks per week had a 56% increased risk of being overweight (BMI more than 24) when compared to those not drinking any diet drinks. People drinking 3 to 10 diet drinks per week had in a 75% increased risk of being overweight and people drinkng more than 21 diet drinks per week had nearly twice the rate of obesity as those not drinking any diet drinks. Researchers concluded by stating,
These findings raise the question whether artificial sweetner use might be fueling--rather than fighting--our escalating obesity epidemic.
OBESITY
Vol. 16(8): 1894-1900, Aug 2008
Dept. of Medicine
University of Texas
Health Sciences
San Antonio, Texas USA
Obesity & Weight Increases
seen in Dogs, Cats & Many Animals
More evidence that obesity is resulting from the environment comes from a major study out of University of Alabama and John Hopkins School of Public Health. Researchers investigated documented weights of cats, dogs, horses, chimpanzees, rhesus monkeys, and even mice and rats over the past 30-40 years. All animals showed trends in increasing weights each decade. For example, their study of 574 female cats found a 13.6% increase in odds of obesity with each passing decade along with a 5.7% increase in body weight per decade. Similar increases were seen in horses and even rats trapped in urban environments in Baltimore, Maryland. In conclusion, the scientists stated the following as a potential explanation,
One set of putative contributors to the human obesity epidemic is the collection of endocrine-disrupting chemicals (endocrine-disruptors), widely present in the environment.
Endocrine Disrupting Chemicals Cause Obesity
The 3 paragraphs below are quoted directly from the 2008 report from the National Institute of Environmental Health Sciences, Developmental Endocrinology and Endocrine Disruptor Section, Research Triangle Park, NC. Again, this is not paraphrased, all text is a direct quote except for the last paragraph under "CHEM-TOX COMMENT."
In this article, data presented showed that the current obesity epidemic cannot be explained solely by alterations in food intake and/or decrease in exercise. The author cited numerous studies where chemicals including pesticides, organophosphates, polychlorinated biphenyls, polybrominated biphenyls, phthalates, bisphenol A, heavy metals and solvents caused weight gain possibly by interfering with weight homeostasis such as alterations in weight-controlling hormones, altered sensitivity to neurotransmitters or altered activity of the sympathetic nervous system.
Environmental chemicals with hormone-like activity can disrupt the programming of endocrine signalling pathways that are established during perinatal life and result in adverse consequences that may not be apparent until much later in life. Increasing evidence implicates developmental exposure to environmental hormone mimics with a growing list of adverse health consequences in both males and females. Most recently, obesity has been proposed to be yet another adverse health effect of exposure to endocrine disrupting chemicals (EDCs) during critical stages of development. Obesity is quickly becoming a significant human health crisis because it is reaching epidemic proportions worldwide, and is associated with chronic illnesses such as diabetes and cardiovascular disease. In this review, we summarize the literature reporting an association of EDCs and the development of obesity, and further describe an animal model of exposure to diethylstilbestrol that has proven useful in studying mechanisms involved in abnormal programming of various oestrogen target tissues during differentiation. Together, these data suggest new targets (i.e. adipocyte differentiation and mechanisms involved in weight homeostasis) of abnormal programming by EDCs, and provide evidence that support the scientific term ‘the developmental origins of adult disease’. The emerging idea of an association of EDCs and obesity expands the focus on obesity from intervention and treatment to include prevention and avoidance of these chemical modifiers.
CONCLUSIONS
The data summarized in this review support the idea that brief exposure early in life to environmental endocrine disrupting chemicals, especially those with oestrogenic activity like DES, increases body weight with age. Whether the results in experimental models can be extrapolated to health hazards in humans as the reproductive abnormalities from the DES mouse model did, remain to be determined but epidemiology studies suggest a link between exposure to environmental chemicals such as polychlorinated biphenyls (PCBs), DDE and persistent organic pollutants with obesity. Further, use of soy-based infant formula containing the oestrogenic component genistein, has also been associated with obesity later in life (Stettler et al., 2005). Use of the DES animal model to study ‘obesogens’ and mechanisms involved in altered weight homeostasis (direct and/or endocrine feedback loops, i.e. ghrelin, leptin, etc.) by environmental endocrine disrupting chemicals is an important basic research tool that may shed light on areas of prevention. Public health risks can no longer be based on the assumption that overweight and obesity are just personal choices involving the quantity and kind of foods we eat combined with inactivity, but rather that complex events including exposure to environmental chemicals during development may be contributing to the obesity epidemic.
Artificial Sweetened Drinks increase Type-2 Diabetes
American J Clinical Nutrition
Vol. 93(6): 1321-1327, Mar 2011
Harvard School of Public Health
|
THE AUSTRALIAN PARADOX
Obesity Increases as Sugar Use in Country Decreases
People in Australia are faced with a mystery: The rate of obesity has increased in Australia 3 fold since 1980. Similar increases have been observed in other countries as well. What is surprising to researchers is that while obesity has continued to increase during this period, the per capita consumption of sugar and high fructose corn syrup has decreased by 16%. In Australia, there was a reduction in sales of nutritively sweetened beverages by 64 million liters from 2002 to 2006 and a reduction in the percentage of children consuming sugar-sweetened beverages between 1995 and 2007. All of this fuels the debate that it is not just an increase in sugar causing the increase rates of obesity.
NUTRIENTS
Vol. 3(4): 491-504, April 2011
Australian Diabetes Council
Dozens of Studies Link Artificial Sweetners
and Metabolic Disorders
This 2013 report reviews results from dozens of studies linking artificial sugars with metabololic defects and diabetes.
Say in Aint So:
Hotdogs, Bacon & Sausage = More Type-1 Diabetes
Pick up a pack of hotdogs, bacon or sausage and you'll often see a chemical in the ingredient listing containing the word nitrate. Nitrate chemicals are convenient for food manufacturers as they help prevent spoilage and allow meat to stay on the shelf for weeks longer in your grocery store. The problem, nitrates react with the acid in your stomach or with high temperatures in the frying pan to form new chemcals called nitrosamines - and these are the bad guys.
So, if your children are anything like mine, they love eating hotdogs, bacon and sausages, however, with this comes the not so good news of increased intake of nitrates and apparently damage to the parts of us which protect us from diabetes.
To determine if eating nitrates in my children's favorite foods increased the risk of diabetes, researchers in Sweden studied 339 children ages 0 to 14 who recently developed type-1 diabetes. They first determined the amount of nitrate foods these children ate along with the amount of nitrate foods eaten by 528 non-diabetic children of similar age, weight and home locations. Once this was calculated, the researchers placed everyone into 3 equal groups according to the amount of nitrate laden food they ate. The one-third of children who ate the lowest amount of nitrates were put into Group 1. Children who consumed the next higher amount of nitrates were labeled as Group 2 and the 1/3rd of children who ate the highest amount of nitrates were put into Group 3. After scientists completed their comparisons and taking into account things such as child age and weight, they found what is called a "significant linear trend for dose response in odds ratios." Without all the fancy talk, this simply means that the more nitrates a child ate - the higher their risk for diabetes. For example, children who ate more hotdogs and bacon etc, who were in the middle nitrate Group 2 had a 1.7 times (70%) higher rate of diabetes. But it didn't stop here; Children who were the truest of fans of hotdogs and bacon and in the highest nitrate Group 3 had a 2.6 times (more than double) higher rate of diabetes than those in Group 1. Regarding just their thoughts on the nitrosamines formed from nitrates, the researchers stated,
...nitrosamine compounds may influence the risk
of developing insulin dependent diabetes in childhood
and significant trends in odds ratios indicate a causal relation
Although not discussed in this study, just thought you might like to know that nitrosamines are also used in the manufacture of cosmetics, thereby increasing the body burden of this chemical in women.
British Medical Journal
Vol. 300(6735), 1302-1306, May 1990
Dept. of Pediatrics
Karolinska Institute
Sachs' Children's Hospital
Stockholm, Sweden
Mystery of the Smoked Mutton Fish
Lucky Pattern Links Nitrates with Diabetes Increase in Boys
Some might call this the mystery of the smoked mutton fish. Well, it all started back in 1980, there were two towns in the country of Iceland that had more than 10,000 residents, but for some unknown reason, they were finding a large number of young boys with diabetes who were all born in the month of October. Let me jump back for a second and say that the Iclanders were a people of tradition and durring the two weeks of their Christmas and New Years celebrations, they would take their beloved mutton fish and smoke them over an open fire. However, beginning in 1940 (about when the rates of type 1 diabetes began to rise in Iceland), the practice of smoking mutton over an open fire was changed to include adding chemical nitrates to the salted fish. Being that Christmas time is quite cold in Iceland, along with the very good spirits everyone was in during the holidays, people were able to spend more time together staying warm. Well, it turns out that 9 months after each yearly mutton smoking tradition, they noticed an increase in boys with type 1 diabetes. Researchers first thought it might have been viruses but that was ruled out. When scientists reproduced the process of making smoked mutton with the same type of nitrates they found the fish contained high concentrations of a nitrate chemical called N-nitroso-compounds. What's interesting, and why it took a while to figure this out, is that no one who ate the fish experienced diabetes - it was only the young boys who were born 9 months later. This would lead one to believe that the nitrate chemicals caused some type of biological problem during pregnancy that increased the rate of diabetes. Bottom line, for those who conceived during the weeks following Christmas, in which they would have eaten considerable amounts of smoked mutton as leftovers, their boys born in October year after year had higher rates of diabetes than boys born in any other month. This strongly suggests that the nitrate type chemicals used in the smoked fish may very well have been responsible. Why this increase wasn't seen in girls is still not known and may be related to the effect the chemical has upon certain hormones. In fact, nitrate is known as a potential endocrine disupting compound and has been found to cause problems in thyroid function and, as shown by the Department of Zoology at University of Florida, can discrupt hormones in young wildlife.
Nitrates in Water Increases Diabetes
Link to Chemical Fertilizers
If nitrates in your hotdogs and mutton wasn't enough to spoil your day, you'll be quite displeased to find that nitrates in your drinking water is also being linked to increasing your chance of getting diabetes. Today's commercial farming practices typically rely on liquid water soluable sources of nitrogen as a fast and easy way to get nitrogen into the soil to grow green leafy plants. Homeowners also apply water soluble nitrogen fertilizers to keep lawns looking prettier than their neighbors. Unfortunately, this highly soluble form of nitrogen increases potential for run-off into nearby streams and rivers and also through the ground and into the water table. Since drinking water is showing increased levels of nitrates, researchers at the University of Leeds wanted to find out if this affected rates of diabetes. The study was done by determining nitrate levels in water for 148 supply zones in Yorkshire England. Results showed that the zones with higher rates of nitrates had higher rates of diabetes after taking into account race, age, weight and other factors.
It should be noted that studies of nitrates in water and diabetes are more controversial than other diabetes promoting chemicals. It should be mentioned that while these studies listed did find a connection between nitrates in water and diabetes, many other studies have failed to do so. This battle is bound to continue and it should be noted that income generated from fertilizer production and sales of nitrate fertilizer for use on farms and residential lawns is enormous. It is recommended that when evaluating these studies you also consider funding sources and any potential conflicts of interest.
A review of over a dozen studies on this topic was published in the October 2016, World Journal of Diabetes.
Diabetologia
Vol. 40(5): 550-556, May 1997
Center for Health Services Research
University of Leeds, UK
World Journal of Diabetes
Vol. 7(18): 433-440, Oct 15, 2016
Shahid Beheshti University
Tehran, Iran
Artificial Sweeteners Cause Glucose Intolerance
https://www.ncbi.nlm.nih.gov/pubmed/23850261
Sucralose - Affects Glucose Levels
https://www.ncbi.nlm.nih.gov/pubmed/23633524
Nature
Vol. 514(7521): 181-186, Oct 2014
Dept of Immunology
Weizmann Institute of Science, Israel
The Controversy Behind the Nightime Insulin Lantus
We all understand how the insulin shots work with each meal; The person eats carbohydrates and then takes insulin to hook-up with the increased glucose that forms as we digest carbohydrates over the next hour or so. The nightime insulin is a little more mysterious. Unlike the fast acting insulin shots taken at breakfast, lunch and dinner, the nightime insulin is intentionally designed to release just small amounts of insulin continuously over a 24 hour period. Its sole purpose is to provide just enough insulin to keep the cells happy that are involved in breathing, heartbeat and our sleeping brain that is dreaming about god knows what. Because of the very small amount of insulin released during each hour, it does practically nothing to reduce your daytime glucose levels. Again, its purpose is to simply make sure there is just enough insulin available for the most basic of body functions. To achieve this time-release effect, scientists created microscopic size crystals that dissolve very slowly at different times over the 24 hour period which means that only a very, very small amount will be available at any given moment over the 24 hours. Although I am just guessing at this, I would assume they make the coating over the insulin of different thicknesses so it dissolves at diffeent times over the 24 hours. As I haven't read any research on the technological process (and they may not publicize this for patent reasons), this is just my guess of a way its desired result could be achieved. In any event, while you may have heard the name Lantus to describe the nightime insulin, it also goes by the more official name of Insulin glargine.
Diabetologia
Vol. 55(1): 51-62, Jan 2012
Dept. of Epidemiology
Erasmus MC
Roptterdam, the Netherlands
| 1895 |
|
|
|
| Age 0-9 |
Black Only |
18 per 100,000 per year |
CDC Chart |
| Age 0-9 |
White Only |
29 per 100,000 per year |
CDC Chart |
| Age 10-19 |
White Only |
32 per 100,000 per year |
CDC Chart |
| Age 10-19 |
Black Only |
45 per 100,000 per year |
CDC Chart |
| Age 10-19 |
All races |
33 per 100,000 per year |
CDC Chart |
| Age 0-9 |
All races |
22 per 100,000 per year |
CDC Chart |
Raising Body Temperature Prevents Type-1 Diabetes
In this study on the effects of raising body temperature,
reseachers stated the following as their purpose for the study.
While type-1 diabetes is an autoimmune disease in which beta-cells of the pancreatic islets are destroyed by cytotoxc T lymphcytes - this condition was shown to be reversed when enhanced natural kill cells controlled the cytotoxic T lymphocytes. Fever-range whole body hyperthermia has also been shown to stimulate natural killer cell cytotoxicity. This led to the hypothesis that fever range whole body hyperthermia can prevent type-1 diabetes onset in NOD mice by a thermally regulated mechanism.
Researchers also stated that natural killer cells in people without diabetes work to remove and reduce cytotoxic T lymphocytes that mistakenly attack the beta-cells in the pancreas. Patients with type-1 diabetes have impaired natural killer cell function so their natural killer cells do not perform as needed, thereby allowing these damaging attacks to on the pancreas to continue. However, raising body temperature to about 103 degrees farenheit has been shown previously to stimulate proper function of natural killer cells. These facts led researchers to test the hypothesis that elevated body temperature could prevent type-1 diabetes in test animals.
Results showed that mice receiving hyperthermia did not develop diabetes while mice not receiving the treatment did develop diabetes. The scientists concluded by stating,
These studies show, for the first time, that mild systemic hyperthermia can prevent the generation of T1D (type-1 diabetes) in a clinically relevant mouse model. Further study of the thermally sensitive aspects of immunoregulation could lead to the development of heatbased therapies for the prevention or treatment of autoimmune diseases.
Higher Body Temperature Improves Diabetes
Type-2 diabetes appears to benefit from elevated temperatures. In this study, mice showed significant improvements in type-2 diabetes insulin resistance when subjected to elevated body termperatures of about 100 degrees F. Mice were exposed to a temperature of 38 degrees celsius (100 degrees farenheit) three times per week for 12 weeks. Temperature was maintained for 30 minutes per treatment. At the end of each treatment, tail snip glucose levels were determined under fasting conditions.
Results showed temperature treated mice showed a significant decease in fasting blood glucose as compared to untreated mice. Plasma insulin levels of untreated mice were significantly higher at age 10 weeks. On the other hand, a 31% reduction of insulin levels in temperature treated mice was also observed demonstrating improved insulin sensitivity. In conclusion, the researchers stated,
Although the mechanisms have not yet been completely investigated, Whole Body Hyperthermia may provide a new therapeutic or preventive modality against obesity-related diseases such as Type 2 Diabetes Mellitus and metabolic or insulin resistance syndrome.
Hair Dyes Possible
Suspect in Autoimmunity
The hair dye ingredient known as p-phenylenediamine (PPD) is used as a dye for dark hair color shades and is made from coal tar. Coal tar includes chemicals such as benzene, phenols and other chemicals. In this study done by the University of Copenhagen, researchers found that the hair dye strongly affects the immune system of mice treated in a "consumer-like" manner. Exposure resulted in immune system T-cell proliferation and production of inteferon-y and interleukin-17 within the lymph nodes. There was also an upgregulation of regulatory T cells and interleukin-10 producing cells. In conclusion the researchers stated,
...it also raises the question whether the immune modulatory effects of hair dyes might influence the development of autoimmune diseases and cancers.
Dogs and Cats Get Diabetes Too!
After unveiling so many things around us that increase the risk of diabetes, we just had to look to see of our 4-legged friends had the same problem. One would think their diabetes rates would also be increasing since they are exposed to many of the same chemicals we are. I have known very few dogs that would turn down a rubber made phthlalate filled chew toy. Apparently, I am not alone in wondering about diabetes in pets, researchers at the Swedish University of Agricultural Sciences investigated type-2 diabetes in cats. After tracking down 396 cat owners with a veterinary diagnosis of diabetes, they asked owners to complete a questionnaire on factors such as housing, diet, activity level, medications and vaccinations. Another group of 1,670 cat owners with healthy cats was used for comparison. When the results came in, they found the expected which was overweight cats had higher rates of diabetes like their human owners. However, what was not expected and very interesting is that cats eating dry food had nearly a 4 times greater risk of diabetes compared to cats eating canned food. Although this wasn't mentioned in the study, it would certainly be interesting to see if dry foods contained larger amounts of chemicals for preventing spoilage of meat-by-products after exposure to air.
J Vet Internal Medicine
December 1, 2016
Dept of Clinical Sciences
Swedish Univ of Agricultural Sciences
Uppsala University
Uppsala, Sweden
Leptin Hormone
When Working Properly our Appetite is Normal
The next time you can't stop thinking about that candy bar after eating a satisfying lunch, you can thank or curse the hormone known as leptin. While somewhat of a cute name - leptin is the Greek word for "thin" and produced primarily by the fat cells in your body to control energy balance, reduce hunger, control metabolism and even improve fertility. Leptin is produced by a gene in our cells and is officially located on chromosome 1p31. If the gene isn't working up to par, we have problems. Leptin is also known to make it easier for your cells to use glucose and improve insulin sensitivity. If our cells are not sensitive to insulin (which means our cells are not responding to insulin) we have symptoms similar to type-2 diabetes. So in summary, you could say this little guy has quite a few job responsibilities and why he needs to be working at 100%.
Under normal circumstances, sometime after eating a meal, leptin is emitted by the fat cells and enters your blood to broadcast to the rest of the body that everything is wonderful. Brain cells in our hypothalmus is one area that has special leptin receptors designed to pick up this leptin message and turn off the desire to eat. That's how it's supposed to work.
Unfortunately, not all men (or women) are created equal in regards to leptin. In a study of people who were obese and simply ate too much, they were found to have a problem known as "leptin resistance" which means their blood contains high levels of leptin but for some reason the hunger desire is not being reduced like it should. So, basically, the "do not eat" message from leptin was being ignored. The next time your larger than average friend is eating like a pro, you can say, it's not your fault - it's leptin - at least it is according to this 2014 study done by researchers at the Laboratory of Metabolism in Guangdong, China.
Physiology Behavior
Vol. 130: 157-169
May, 2014
Laboratory of Metab.
Guangdong Pharm
U.
China
Malfunction of Obesity Gene and Type 2 Diabetes
Makes us Eat at the Wrong Time
It's somewhat comforting for those of us blessed with more real estate around our middle to know that thin people aren't smarter - they just get a lot of help from proper function of the hormone leptin and leptin receptors in controlling appetite and metabolism. In a review of studies on this topic, researchers in Israel and at Harvard Medical School reported on studies showing people with type-2 diabetes had lower leptin expression in fat tissue and also lower serum leptin levels as well. Because of this insight, researchers at the Harbin Medical University in China wanted to know if there was a difference in genes controlling leptin and the leptin receptors in people with type-2 diabetes.
After looking over a dozen studies have been done on this topic they found there was in fact an agreement on several points showing abnormalities in some genes. I apologize for the medical terminology, but in conclusion they stated,
To the best of our knowledge, this is the first meta-analysis to investigate the association of LEPR gene with T2DM. Our results suggested that the polymorphism rs1137101 (p.R223Q) has strong association with T2DM susceptibility. More studies in larger cohort and functional analyses of LEPR are required to reinforce the results and elucidate its biological roles in diabetes.
Journal of Diabetes Research
Vol 2016 (2016)
Harbin Medical University
Dept of Endocrinology
China
Front Neuroendocrinology
Vol. 31(3): 377-393
Beth Israel D Med Ctr
Harvard Med School
Boston, MASS, USA
 The percentage of the U.S. population with diabetes has increased dramatically over the past 20 years and is increasing faster with each passing year. In the following report, we will provide clear and convincing evidence that the main force driving the rising rates of diabetes is not an increasing elderly population or the increase in obesity, but is occurring from something else.
The percentage of the U.S. population with diabetes has increased dramatically over the past 20 years and is increasing faster with each passing year. In the following report, we will provide clear and convincing evidence that the main force driving the rising rates of diabetes is not an increasing elderly population or the increase in obesity, but is occurring from something else.
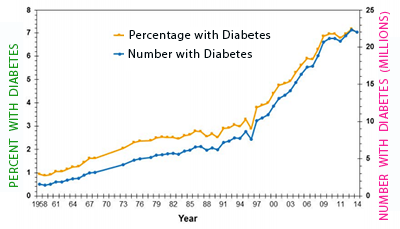 Here's some numbers that should wake you up - when looking at the latest numbers from 2012, researchers found that 14% of the adult U.S. population had either doctor diagnosed diabetes or undiagnosed diabetes. Also using 2012 numbers, the
Here's some numbers that should wake you up - when looking at the latest numbers from 2012, researchers found that 14% of the adult U.S. population had either doctor diagnosed diabetes or undiagnosed diabetes. Also using 2012 numbers, the 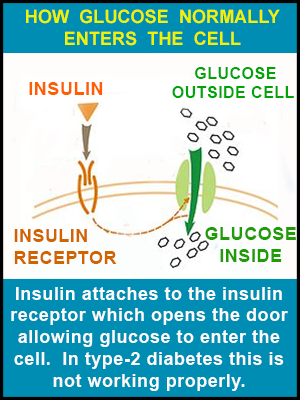 Before letting you go, let me explain this in a way that will paint a picture for better understanding type-2 diabetes. The cells in your body are basically a round spherical shape. Coated along the cell surface are a number of doors - some are marked "INSULIN" and others "GLUCOSE." Your beta-cells in your pancreas produce insulin which enters the blood traveling to all different parts of your body. When Mr. Insulin comes to his door - the door-keeper immediately recognizes Mr. Insulin and let's him inside. Once inside, the door-keeper yells to his friend guarding the glucose door and says, "Mr. Insulin is here, you can now let in Mrs. Glucose." The glucose doors open and Mrs. Glucose (being the life of the party she is), gets everybody in a great mood and things are wonderful! The problem with type-2 diabetes appears to lie with the door-keepers as they don't always recognize and allow Mr. Insulin through the door and into the cell. Maybe some kind of grudge from a previous party, but the bottom line is the door-keeper (officially the insulin receptor) resists letting Mr. Insulin inside so he is left out in the cold - and if Mr. Insulin can't get in his door then Mrs. Glucose can't get in her door either. For those wishing to research this further, the scientific term for the insulin door is the insulin receptor and for glucose it is the glucose transporter. Type 2 diabetes is responsible for about 90% of all diabetes cases and typically raises its ugly self in older individuals, although since the 1990's, it has been occurring at higher and higher rates in children 10-18 years old.
Before letting you go, let me explain this in a way that will paint a picture for better understanding type-2 diabetes. The cells in your body are basically a round spherical shape. Coated along the cell surface are a number of doors - some are marked "INSULIN" and others "GLUCOSE." Your beta-cells in your pancreas produce insulin which enters the blood traveling to all different parts of your body. When Mr. Insulin comes to his door - the door-keeper immediately recognizes Mr. Insulin and let's him inside. Once inside, the door-keeper yells to his friend guarding the glucose door and says, "Mr. Insulin is here, you can now let in Mrs. Glucose." The glucose doors open and Mrs. Glucose (being the life of the party she is), gets everybody in a great mood and things are wonderful! The problem with type-2 diabetes appears to lie with the door-keepers as they don't always recognize and allow Mr. Insulin through the door and into the cell. Maybe some kind of grudge from a previous party, but the bottom line is the door-keeper (officially the insulin receptor) resists letting Mr. Insulin inside so he is left out in the cold - and if Mr. Insulin can't get in his door then Mrs. Glucose can't get in her door either. For those wishing to research this further, the scientific term for the insulin door is the insulin receptor and for glucose it is the glucose transporter. Type 2 diabetes is responsible for about 90% of all diabetes cases and typically raises its ugly self in older individuals, although since the 1990's, it has been occurring at higher and higher rates in children 10-18 years old.
 In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
In December, 2013, this child was diagnosed with type-1 diabetes with a glucose level of 692 mg/dl and glucose in urine. He also tested positive for GAD autoantibodies (1280 IU/ml). He was placed on an insulin therapy of 21 units for six meals containing 210 grams of carbohydrates. He was on conventional insulin therapy for six weeks. Although he followed the prescribed diabetes diet and insulin treatment, his glucose levels fluctuated considerably. This resulted in his parents looking for alternative treatments.
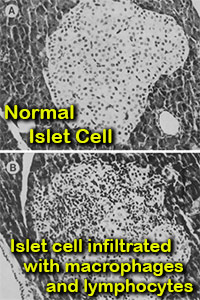 Macrophages are a type of white blood cell in the immune system.
In conclusion, the scientists stated, Along with cells called dendritic cells, macrophages are number 1 among cells that present signals (antigens) to other cells to mount an attack. Researchers in this study found an interesting observation among mice genetically prone toward diabetes type-1. When mice were exposed to a compound known to cause diabetes, the islets in their pancreas (islets hold insulin producing beta-cells) became flooded with macrophages and other immune system cells in a process known as insuliltis (see picture). They also found that by reducing macrophages (through exposure to silica), there was a dramatic decrease in function and numbers of T lymphocytes and natural killer cells - resulting in prevention of the pancreas beta-cell destruction. The authors quoted other studies showing that natural killer cells and helper and cytotoxic T lymphocytes are actively involved in the destruction of islet cells (paragraph 3, Pg.585).
Macrophages are a type of white blood cell in the immune system.
In conclusion, the scientists stated, Along with cells called dendritic cells, macrophages are number 1 among cells that present signals (antigens) to other cells to mount an attack. Researchers in this study found an interesting observation among mice genetically prone toward diabetes type-1. When mice were exposed to a compound known to cause diabetes, the islets in their pancreas (islets hold insulin producing beta-cells) became flooded with macrophages and other immune system cells in a process known as insuliltis (see picture). They also found that by reducing macrophages (through exposure to silica), there was a dramatic decrease in function and numbers of T lymphocytes and natural killer cells - resulting in prevention of the pancreas beta-cell destruction. The authors quoted other studies showing that natural killer cells and helper and cytotoxic T lymphocytes are actively involved in the destruction of islet cells (paragraph 3, Pg.585).
 While the chemical BPA has been linked with increasing obesity in a number of studies, this is the first study we've seen that was able to measure how much fat cells actually grew after exposure to BPA. Since humans could not be involved in a study of this design, scientists took cells from mice that normally grow into fat cells - scientists call them adipocytes. Since adipocytes and fat cells are the same thing we'll go with "fat cells" to save energy in pronunciation. The experiment worked like this: Scientists in Italy at the Federico University of Naples first treated a group of mouse pre-fat cells (called fibroblasts) with low levels of BPA for 2 weeks. The level of BPA is said to be what most of us are exposed to during our daily routine. On the beginning of the 15th day of the experiment, the pre-fat cells were placed into six separate plates for growing and observaton. At the end of 24 hours on day 16, the number of cells were counted and photographed. This was done again on day 17 and day 18.
While the chemical BPA has been linked with increasing obesity in a number of studies, this is the first study we've seen that was able to measure how much fat cells actually grew after exposure to BPA. Since humans could not be involved in a study of this design, scientists took cells from mice that normally grow into fat cells - scientists call them adipocytes. Since adipocytes and fat cells are the same thing we'll go with "fat cells" to save energy in pronunciation. The experiment worked like this: Scientists in Italy at the Federico University of Naples first treated a group of mouse pre-fat cells (called fibroblasts) with low levels of BPA for 2 weeks. The level of BPA is said to be what most of us are exposed to during our daily routine. On the beginning of the 15th day of the experiment, the pre-fat cells were placed into six separate plates for growing and observaton. At the end of 24 hours on day 16, the number of cells were counted and photographed. This was done again on day 17 and day 18.
 Results showed a number of major differences between fat cells exposed to BPA and fat cells not exposed to BPA. First, fat cells exposed to BPA were only able to use half as much glucose as those not exposed to BPA, thereby giving evidence of insulin resistance.
Results showed a number of major differences between fat cells exposed to BPA and fat cells not exposed to BPA. First, fat cells exposed to BPA were only able to use half as much glucose as those not exposed to BPA, thereby giving evidence of insulin resistance.
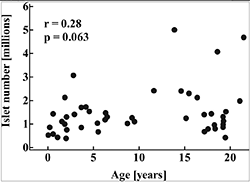
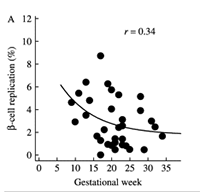
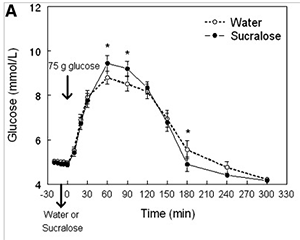 Studies on artificial sweeteners are a bit tricky. While some show problems with worsening glucose or diabetes symptoms - others do not. For example, in a study reported in the October 2017 journal
Studies on artificial sweeteners are a bit tricky. While some show problems with worsening glucose or diabetes symptoms - others do not. For example, in a study reported in the October 2017 journal